Endodontic retreatment: expect the unexpected
09/04/2024
Fellow
Warning: Undefined variable $post in /var/www/vhosts/styleitaliano-endodontics.org/endodontics.styleitaliano.org/wp-content/plugins/oxygen/component-framework/components/classes/code-block.class.php(133) : eval()'d code on line 2
Warning: Attempt to read property "ID" on null in /var/www/vhosts/styleitaliano-endodontics.org/endodontics.styleitaliano.org/wp-content/plugins/oxygen/component-framework/components/classes/code-block.class.php(133) : eval()'d code on line 2
The goal of an endodontic treatment is to disinfect the root canal system. This will facilitate the resolution of inflammation and the alleviation of symptoms. Failure to achieve this goal means that parts of the root canal system will not be thoroughly cleaned and will carry on containing a significant population of bacteria. This fact will sustain infection and jeopardize the outcome of the treatment.
In retreatment cases, the clinician has to deal with many mishaps such are underfilled, missed and obstructed canals as also with iatrogenic damages as separated instruments and perforations. Underfilled and missed canals constitute the main reasons for endodontic failures (>30%).Especially perforations can be a real challenge since it can strongly reduce the success rate, being responsible for 3-4 % of endodontic failures and extraction of endodontically treated teeth. Size, location and duration since treatment are the main factors influencing the outcome of perforation treatment, while secondary factors can be the material used and the existence of radiolucency.

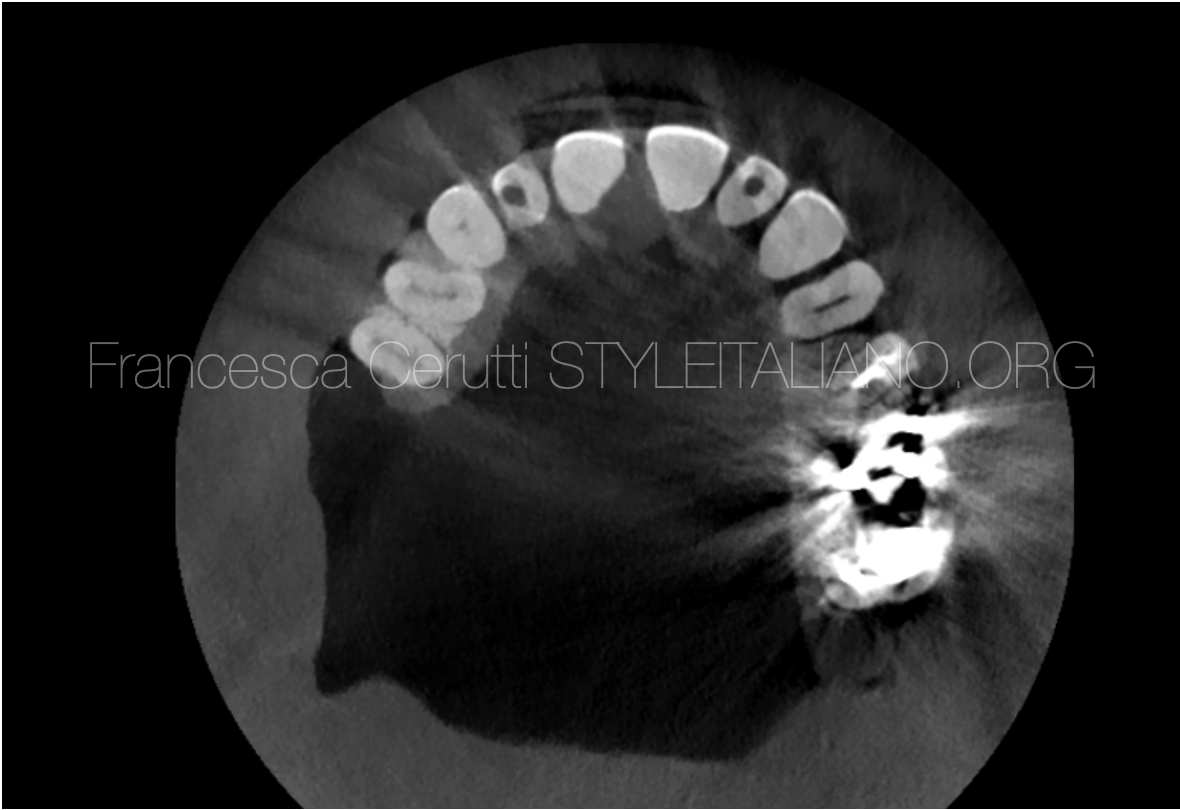
Fig. 1
A 52-year-old male patient was referred to my practice for an endodontic retreatment on tooth 26. The patient had experienced pain and swelling and he was under antibiotics (Augmentin 625mg). The tooth was sensitive on percussion and palpation and was periodontally healthy.
The initial x-ray shows three underfilled canals, a large periapical lesion and a big radiolucency in the furcation area. Periodontal examination didn’t reveal any loss of attachment neither a furcation involvement.
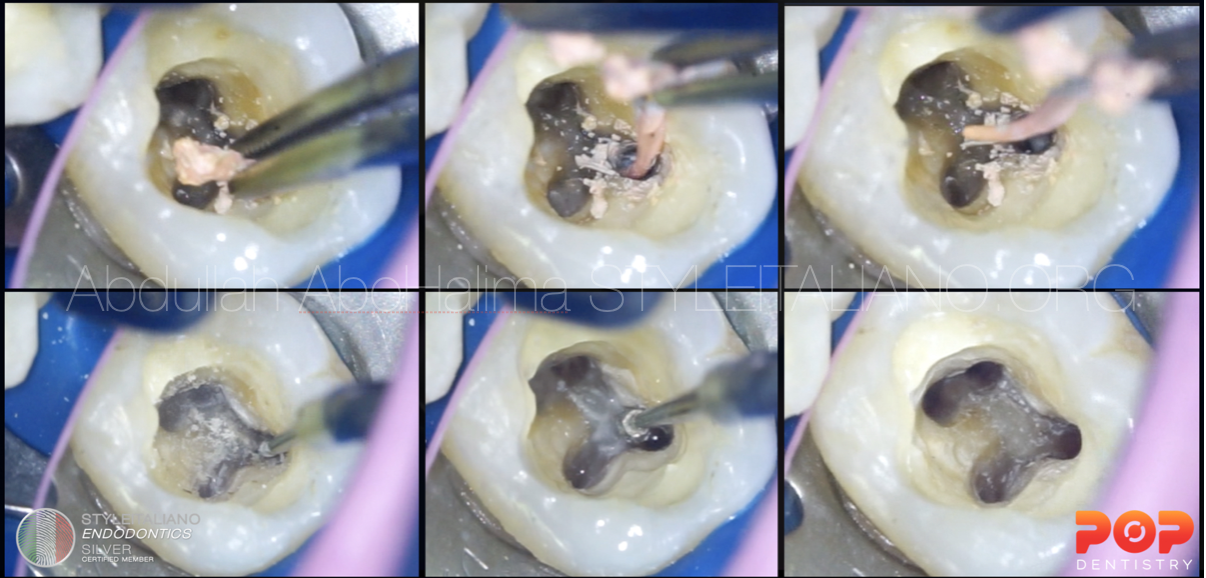
After anesthesia and proper isolation, a minimal access cavity was made using diamond burs and 330 steel burs. The pulp chamber was adequately enlarged preserving at the same time precious peri-cervical dentine.
Four canals were identified (MB1, MB2, DB and P), three of them being treated (MB1,D and P) and one (MB2) was untreated. But the most important finding was a perforation, with profound bleeding and exudate, mesial and buccal to the palatal canal, having the size of a diamond bur. This perforation has been untreated for 2 months which was the time from the primary endodontic treatment. The favorable element about this perforation was that it was not in communication with the oral cavity.
Due to the size of the perforation, it was decided to deal with it before the retreatment of the canals because I did not want to introduce more debris and bacteria to the perforation.
The fact that there was bone loss in the furcation area, increased the need of a barrier to prevent the extrusion of the sealing material. For that reason, the perforation area was cleaned with Chlorhexidine 0,2% and the furcation defect was filled with Periocline, an antibiotic paste (Minocycline) which is successfully used in periodontal defects. After this, a collagen sponge was placed as a barrier and the perforation was sealed with Bioceramic putty. A slightly moistened cotton pellet was placed over the material for 24 hours in order to prevent cotton from being stuck to the material and a new appointment was made to proceed with the retreatment.
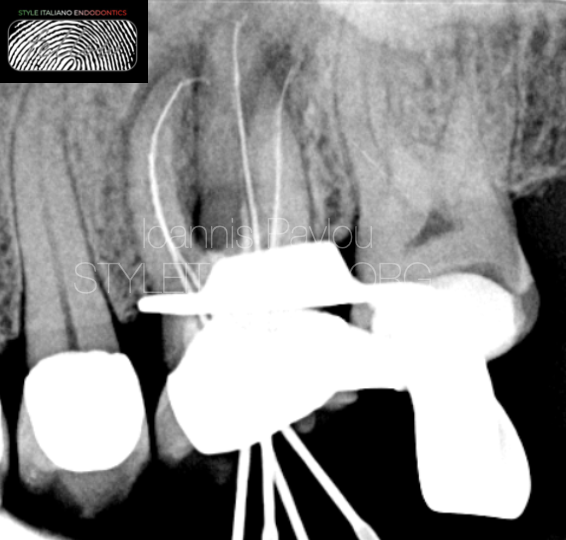
Fig. 2
At the second appointment, the orifices of the canals were enlarged with Gates Glidden for the already treated canals or with orifice opener for the MB2. A cycle of irrigation was performed at this stage in order to reduce the bacterial load and prevent more microbes introduced to the untreated parts.
The canals were negotiated with no8 and 10 D-finders to the apex with the aid of an apex locator. The working length was verified with an interim x-ray with files at zero point.
The pathway was further enlarged with the use of no15 D-finder and no20 K-file. For the shaping and finishing of the canals AF F One rotary instruments were used. This line with R-wire technology and the flat design on one side, presents easier instrumentation and increased resistance to cyclic and torsional fatigue. The canals was instrumented up to 35.04, verifying the extraction of clean dentinal debris. The chemomechanical disinfection was completed with copious irrigation of EDTA 17% (3 mins) and NaOCl 5,25% (10ml per canal, 10 mins) with the aid of ultrasonic activation (Ultra-X). The canals were dried with intracanal suction and paper points. Intracanal medicament was placed for 7 days (Calcipast).
At the third visit one week later, patient confirmed a great reduction of symptoms, but he was still feeling tender to percussion and chewing. It was decided to proceed with a new cycle of irrigation and placement of intracanal medicament for one more week. The intracanal medicament was removed with irrigation and ultrasonic activation. Instrumentation to the established working length with the master file for each canal was executed. Canals were dried and Ledermix, an antibiotic paste successfully used in persistent endodontic infections with great results in the reduction of interappointment symptoms, was placed in the canals and slightly extruded from the apex.

Fig. 3
One week later, patient reported complete resolution of symptoms. Intracanal medicament was removed with copious irrigation of NaOCl 5.25% under ultrasonic activation (Ultra-X), saline and final irrigation with 17% EDTA. Canals were dried with intracanal suction and paper points. An interim x-ray (cone fit) was done to verify the extent of obturation. Obturation was done with single cones and Bioceramic sealer (Neosealer, Avalon). Patient was sent back to the referral dentist for permanent restoration. Although the fit and margins of the existing crown were not satisfactory, it was decided to postpone the new crown until the follow-up and the verification of healing, since the patient is living abroad.

Fig. 4
Post operative X-ray

Fig. 5
About the author:
Ioannis Pavlou
I graduated as a Certified Dental technician in 1995 from the Technological Educational Institution of Athens. In 2002 I completed my dental studies at the Aristotle University of Thessaloniki. I worked and studied in the UK for 8 years completing a series of postgraduate studies, the most important being the Postgraduate Diploma in Endodontics (Queen Mary, London) and the Postgraduate Diploma in Periodontology (University of Central Lancashire). I returned to Greece in 2010 and since 2015 I have been the principal of a clinic limited in Endodontics and Periodontics. In 2022 I completed the MSc in Prosthodontics at the University of Siena with a special interest in bruxism and TMD.
Conclusions
Endodontic retreatments present many problems that every clinician needs to overcome in order to reduce if not eliminate the bacterial load within the root canal system as also to adequately seal the tooth to prevent extrusion of bacteria to the periapical and furcation areas. These two targets are necessary requirements during an endodontic treatment for the resolution of the inflammation and the promotion of healing in the surrounding hard and soft tissues.
Bibliography
- Clauder T. (2022) Present status and future directions – Managing perforations. Int Endod J, 55(Suppl. 4), 872–891. Available from: https://doi.org/10.1111/iej.13748
- Olcay, K., Ataoglu, H. & Sema Belli, S. (2018) Evaluation of related factors in the failure of endodontically treated teeth: a cross-sectional study. Journal of Endodontics, 44, 38–45.
- Atila, Deniz and Vignesh Kumaravel. “Advances in antimicrobial hydrogels for dental tissue engineering: regenerative strategies for endodontics and periodontics.” Biomaterials science (2023): n. pag.
- Hegde VR, Jain A, Patekar SB. Comparative evaluation of calcium hydroxide and other intracanal medicaments on postoperative pain in patients undergoing endodontic treatment: A systematic review and meta-analysis. J Conserv Dent. 2023 Mar-Apr;26(2):134-142. doi: 10.4103/jcd.jcd_501_22. Epub 2023 Mar 16. PMID: 37205901; PMCID: PMC10190086.
- Chybowski, Elizabeth A. et al. Clinical Outcome of Non-Surgical Root Canal Treatment Using a Single-cone Technique with Endosequence Bioceramic Sealer: A Retrospective Analysis Journal of Endodontics, Volume 44, Issue 6, 941 - 945 b