Endodontic management of tooth 2.5 in a patient taking bisphosphonates.
18/04/2025
Fellow
Warning: Undefined variable $post in /home/styleendo/htdocs/styleitaliano-endodontics.org/wp-content/plugins/oxygen/component-framework/components/classes/code-block.class.php(133) : eval()'d code on line 2
Warning: Attempt to read property "ID" on null in /home/styleendo/htdocs/styleitaliano-endodontics.org/wp-content/plugins/oxygen/component-framework/components/classes/code-block.class.php(133) : eval()'d code on line 2
Bisphosphonate-related osteonecrosis of the jaws (BRONJ) is seen occasionally in bisphosphonate-receiving patients for several medical conditions such as osteoporosis, Paget’s disease or metastatic cancer. The term BRONJ was later changed to MRONJ (medication-related osteonecrosis of the jaws), including the growing number of gnathic osteonecrosis cases associated with other antiresorptive (denosumab) and antiangiogenic medications.
Pre-existing pathological inflammatory conditions, such as Apical Periodontitis (AP), have been speculated to be an additional risk factor that increases MRONJ development.
As Bisphosphonates (BPs) are known to activate inflammatory signals, it is known that the presence of some local pathological inflammatory condition (e.g. AP) might worsen the wound healing process of the bone following tooth extraction.
The following clinical case shows a 82 years old female patient under Alendronate (70 mg 1 times a week for 2 years), with chronic apical abscess on 2.5 tooth and pus drainage. Provided that the presence of a chronic apical abscess is a condition that could trigger osteonecrosis, the treatment plan should aim to resolve the pathology as conservatively as possible.
At first moment, endodontic retreatment was performed, and the infection seemed to be solved.
After 9 months the sinus tract with pus drainage reoccured. This is the reason why it was decided to perform an endodontic microsurgery after 1 year of follow-up.
The following images show the specific clinical case and the pharmacological therapies prescribed to the patient.

Fig. 1
A 82-year-old female patient went for a dental check up, referring as chief complain pain during chewing associated with tooth 2.5. After clinical examination, the tooth showed a positive response to percussion test, with no pathological periodontal probing depths and presence of sinus tract. The preoperative periapical x-ray revealed inadequate endodontic treatment, an AP, and a probable perforation in the distal part of the root. Based on the clinical and radiographic findings, diagnosis and pulp status were previously treated tooth with chronic apical abscess.
Since the patient had been taking bisphosphonates for two years, it was decided to perform an endodontic retreatment as first line therapy. Furthermore, the patient request was to save the prosthetic bridge.
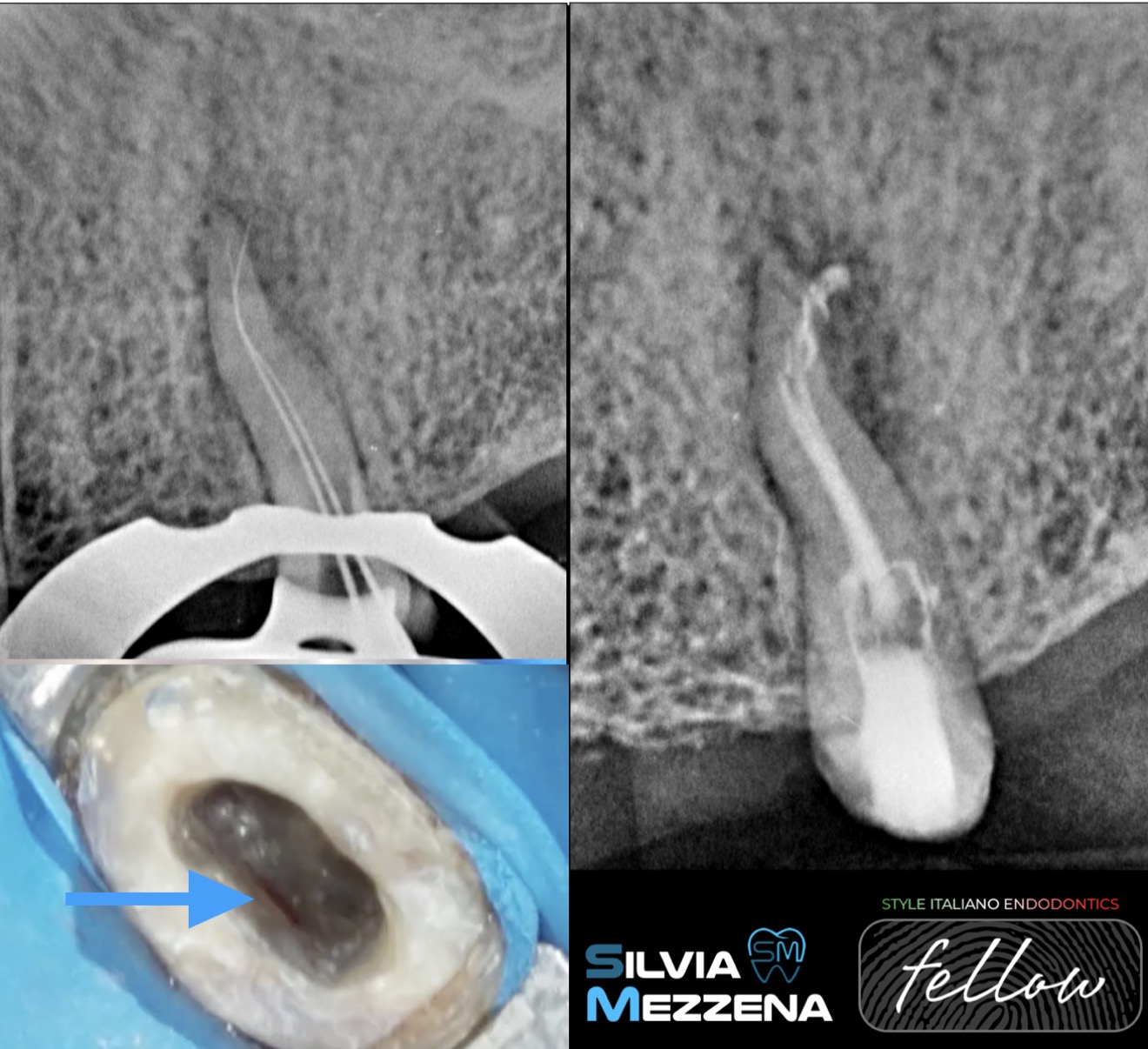
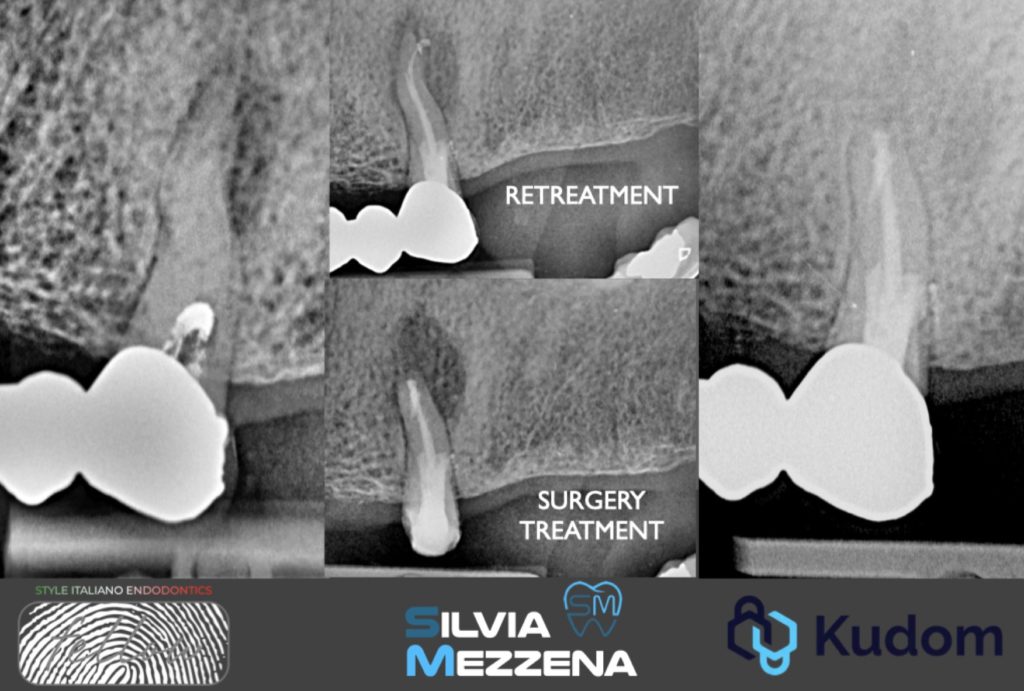
Fig. 2
Fig.2: Secondary Root Canal Treatment.
One visit retreatment was performed. The prosthetic bridge was easily removed, and after the access opening, an unknown sealer in the tooth chamber was mechanically removed with #1 Munce bur.
The perforation in the distal part of pulpal chamber was found, but it was decided to perform the canals instrumentation before the fixing of the defect. For this phase, the gold rotary system was chosen, and the shaping of root canals reached the ISO 20.07 taper (F1).
Irrigation: NaOCL 5%, EDTA 17% with Ultrasonic Activation were used.
Obturation: Zinc Oxide Eugenol Based RCT Sealer and thermafil obturators were chosen to fill the root.
The post-operative x-ray revealed the presence of different ramifications of the apical part, and the root canal filling seemed inadequate in the lingual root, probably for the presence of an anatomical block (thermafil? k-file?).
Since removing a potential separated instrument in the apical part of the root would have further weakened the dental structure, the strategy decision for an accurate follow up has been taken.

Fig. 3
Subsequently, the perforation was closed with a calcium silicate-based cement in putty form. At the second appointment, after verifying the hardening of the material, the post-endodontic restoration was performed using a fiber post in the lingual root and composite material.
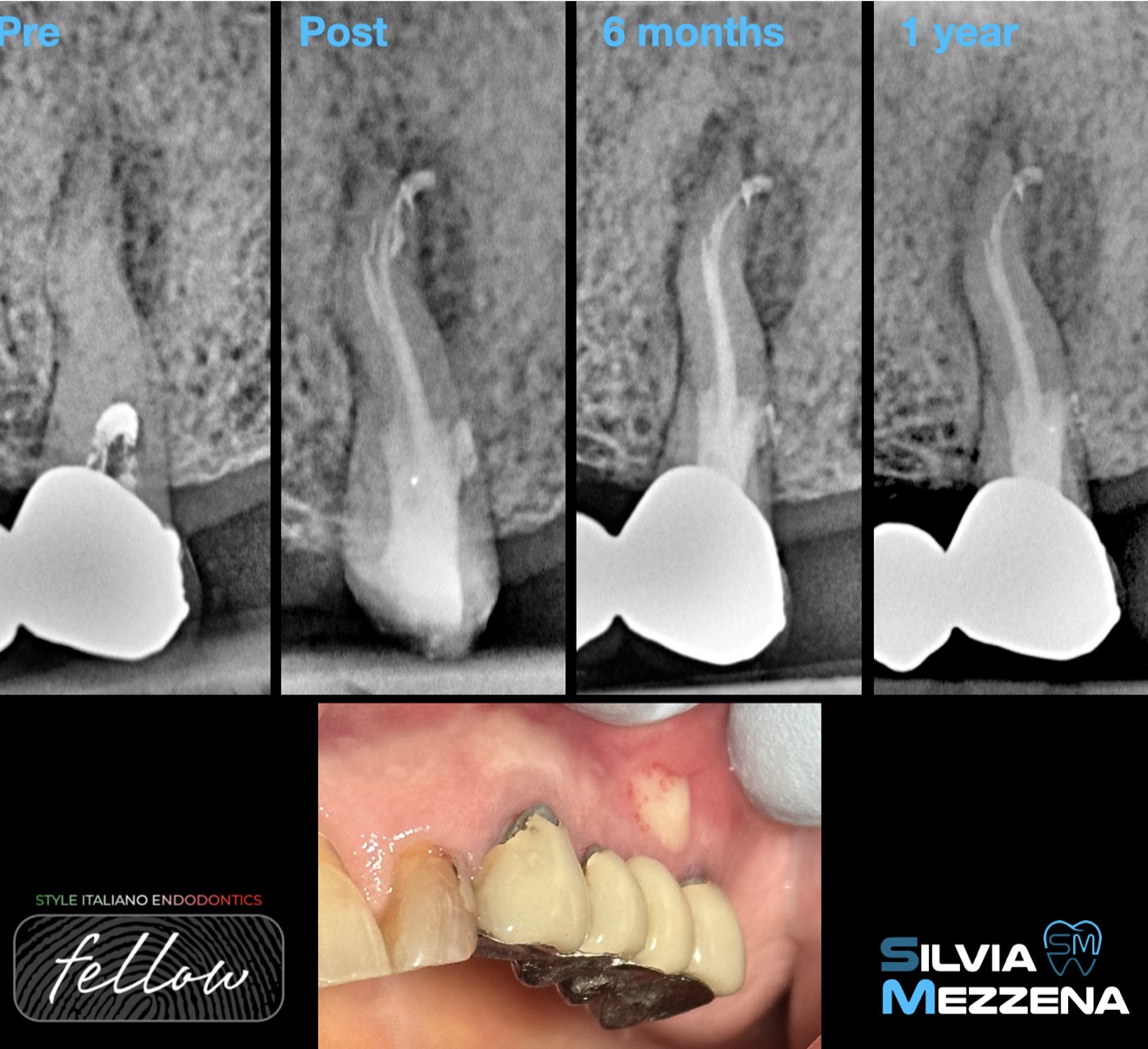
Fig. 4
The tooth stayed asymptomatic with the regression of the sinus for the first 6 months.
Unfortunately, pus drainage from the sinus tract reoccured after 9 months, so the bisphosphonate therapy was interrupted. The radiographic follow-up revealed a worsening of AP after one year, and endodontic microsurgery treatment was planned.
A pharmacological therapy was prescribed as follows: Amoxicillin + Clavulanic acid 1g + Metronidazole 250 mg (1 tablet of each every 12 hours starting 3 days before the procedure and continuing for an additional 7 days after the surgery).
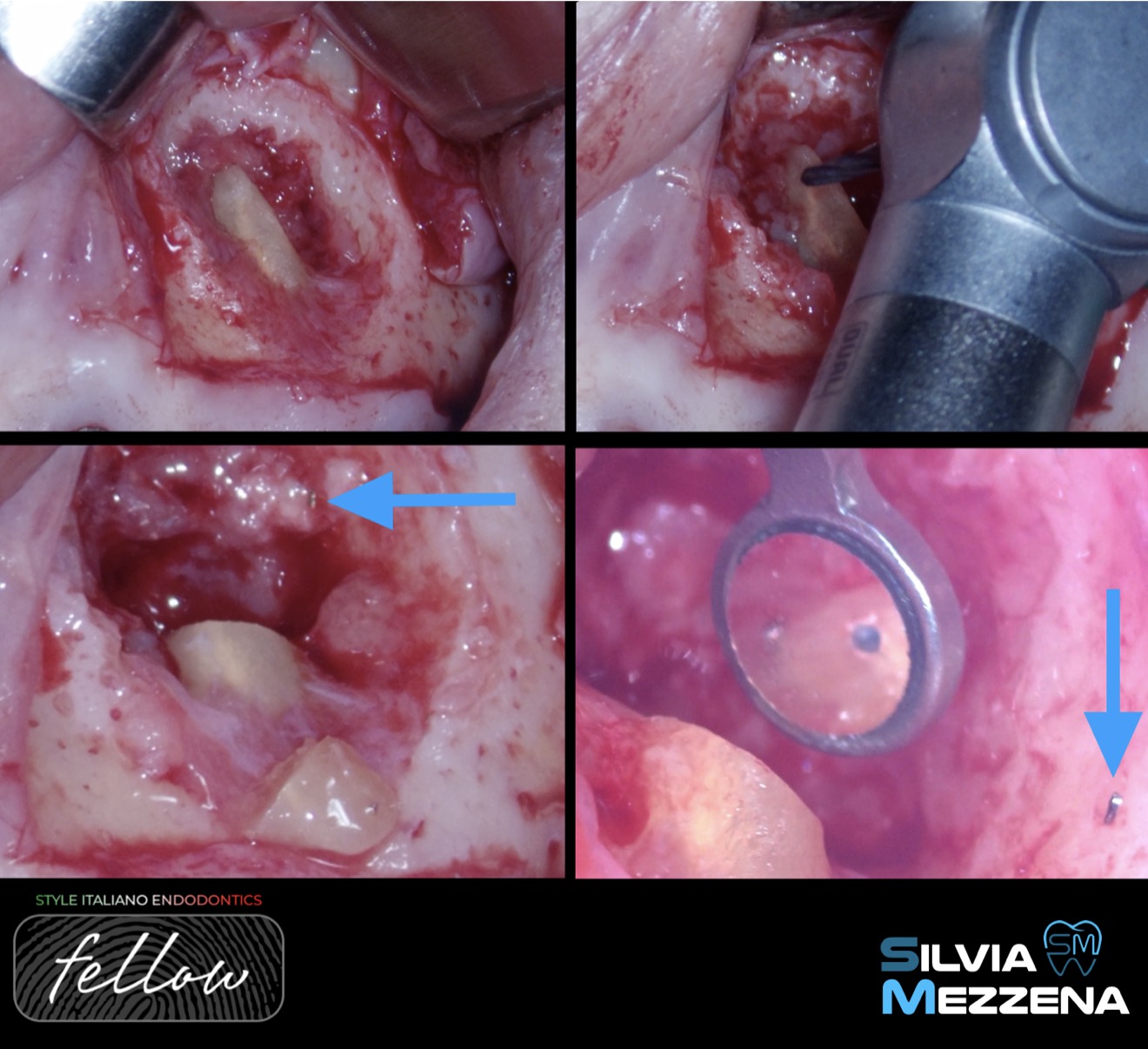
Fig. 5
The surgery was performed under local anesthesia using 1:50,000 Lidocaine. A full-thickness mucoperiosteal flap with a mesial and distal releasing incisions was carefully elevated to obtain the adequate access to the treatment area. Since the granulation tissue was immediately visible once the cortical bone was exposed, osteotomy was not necessary.
After the removal of granulation tissue, the apicoectomy was performed with a Lindemann bur.
The broken K-file instrument can be seen in the images below, after the apex section (blue arrow). Additionally, the two sealed root canals are represented: the vestibular one sealed with Thermafil and the lingual one with the broken instrument inside.

Fig. 6
Retropreparation was performed with ultrasonic tips, creating a cavity suitable for sealing with a premixed bioceramic putty cement. The flap was repositioned and sutured with non-resorbable 4-0 PTFE sutures to ensure a tight closure.
The patient received all postoperative and take-home care hygiene instructions, including the use of 0.20% chlorhexidine mouthwash + 1% chlorhexidine periodontal gel, three times/day for 15 days after oral hygiene.

Fig. 7
The X-rays show the preoperative and post-surgery condition.
The pictures of the tissues represent the situation at 7 and 30 days.

Fig. 8
After 6 months from the surgery, the tooth was asymptomatic and functional. An initial healing of AP was already evident, and the consent to restart the therapy with BPs was given to the patient. The fistula and pus drainage were no longer present.
The image below shows how the tissues are presenting after one year and a half.

Fig. 9
Conclusions
After 6 months from the surgery, the tooth was asymptomatic and functional. An initial healing of AP was already evident, and the consent to restart the therapy with BPs was given to the patient. The fistula and pus drainage were no longer present.
The image below shows how the tissues are presenting after one year and a half.
Bibliography
-Ruggiero, Salvatore L. et al. American Association of Oral and Maxillofacial Surgeons Position Paper on Medication-Related Osteonecrosis of the Jaw—2014 Update. Journal of Oral and Maxillofacial Surgery, Volume 72, Issue 10, 1938-1956
-Weinstein RS, Roberson PK, Manolagas SC. Giant osteoclast formation and long-term oral bisphosphonate therapy. N Engl J Med. 2009;360(1):53–62. doi: 10.1056/NEJMoa0802633.
-Adami S, Bhalla AK, Dorizzi R, Montesanti F, Rosini S, Salvagno G, et al. The acute-phase response after bisphosphonate administration. Calcif Tissue Int. 1987;41(6):326–331. doi: 10.1007/BF02556671.
-Song M, Alshaikh A, Kim T, Kim S, Dang M, Mehrazarin S, Shin KH, Kang M, Park NH, Kim RH. Preexisting Periapical Inflammatory Condition Exacerbates Tooth Extraction-induced Bisphosphonate-related Osteonecrosis of the Jaw Lesions in Mice. J Endod. 2016 Nov;42(11):1641-1646. doi: 10.1016/j.joen.2016.07.020. Epub 2016 Sep 13. PMID: 27637460; PMCID: PMC5085836.
-Tiwari UO, Chandra R, Tripathi S, Jain J, Jaiswal S, Tiwari RK. Comparative analysis of platelet-rich fibrin, platelet-rich fibrin with hydroxyapatite and platelet-rich fibrin with alendronate in bone regeneration: A cone-beam computed tomography analysis. J Conserv Dent. 2020 Jul-Aug;23(4):348-353. doi: 10.4103/JCD.JCD_228_20. Epub 2021 Jan 16. PMID: 33623234; PMCID: PMC7883795.
-Tsesis I, Rosen E, Taschieri S, Telishevsky Strauss Y, Ceresoli V, Del Fabbro M. Outcomes of surgical endodontic treatment performed by a modern technique: An updated meta-analysis of the literature. J Endod. 2013;39:332–9. doi: 10.1016/j.joen.2012.11.044.
-Peñarrocha M, Martí E, García B, Gay C. Relationship of periapical lesion radiologic size, apical resection, and retrograde filling with the prognosis of periapical surgery. J Oral Maxillofac Surg. 2007;65:1526–9. doi: 10.1016/j.joms.2006.10.058.
-Rosini S, Rosini S, Bertoldi I, Frediani B. Understanding bisphosphonates and osteonecrosis of the jaw: uses and risks. Eur Rev Med Pharmacol Sci. 2015 Sep;19(17):3309-17. PMID: 26400539.