
ENDO-PERIO LESIONS: SIMPLIFIED CLASSIFICATION
01/11/2024
Diana Ibrahim ElSanour
Warning: Undefined variable $post in /home/styleendo/htdocs/styleitaliano-endodontics.org/wp-content/plugins/oxygen/component-framework/components/classes/code-block.class.php(133) : eval()'d code on line 2
Warning: Attempt to read property "ID" on null in /home/styleendo/htdocs/styleitaliano-endodontics.org/wp-content/plugins/oxygen/component-framework/components/classes/code-block.class.php(133) : eval()'d code on line 2
The Periodontal and pulpal spaces may communicate through various portals, such as root canal foramen, dentinal tubules, and even crack lines, through which bacteria and its irritants may trigger inflammatory responses in surrounding tissues (1).
Persistent infection in the pulp tissue leads to secondary infection and breakdown of tissues in the periodontium. Conversely, severe periodontal disease may initiate or exacerbate inflammatory changes in the pulp tissue. This happens through anatomical routes, allowing for communication between the two spaces (1).
The main route of communication is the apical foramen. Advanced pulpitis will lead to pulp necrosis, accompanied by inflammatory bone resorption at the root apex, causing apical periodontitisor an apical abscess andknown as retrograde periodontitisrepresenting periodontal tissue breakdown from an apical to a coronal direction. While orthograde periodontitis, results from a sulcular infection and identified as a periapical radiolucency (PARL) (1).
The second route of periodontal/pulpal communications is lateral or accessory canals. With prevalence 59.5% of maxillary second premolars; 78.2% of those are located in the apical regions. While mid-root and cervical regions, with reduced frequencies at 16.2% and 4.0%, respectively (1). Kirkham (1975) reported that only 2% of teeth possessed accessory canals within the periodontal pocketsamong those extracted due to severe periodontal disease.Thus, it’s rare that primary periodontal infections will reach the dental pulp through accessory canals (2).
The third route of communication is the dentinal tubules. Bacterial colonizationin the tubules from infected root canals and bacterial invasion into dentinal tubules from the periodontal pocket has been reported (3).
In addition, there are instances in which communication is non-anatomic as in cases of iatrogenic defects such as vertical root fractures (VRFs), tooth perforations and resorptive defects (1).
The terminology of ‘periodontal-endodontic (endodontic-periodontal) lesions’ often refered to as ‘endo-perio (perio-endo) lesions.’ Many authors have defined those lesions as primary endodontic or primary periodontal lesions causing secondary periodontal or secondary endodontic involvement, respectively, that can also be presented independently and may coalesce (4). These lesions may require endodontic or periodontal treatment or a combined interdisciplinary treatment approach. In 1919 Turner and Drewfirst described the effect of periodontal disease on the pulp (5). In1964 Simring and Goldberg described the relationship between periodontal and pulpal disease. (they are estimated to cause 50% of tooth mortality). Though EPLs are encountered difficult to the clinician in diagnosis and complicate the treatment (5). In Abbott and Salgado 2009highlighted that endo-perio lesions should be limited to those teeth that have both independent endodontic and periodontal diseases occurring at the same time, which can be with or without communication (6). Ahmed (7) defined endo-perio lesions as the dependent and/or independent involvement of the pulp (or the pulp space in case of endodontically treated teeth) and periodontal tissues of an individual tooth.
Classification of a disease (by its clinical presentation) is fundamental; the identification of its causes allows appropriate treatment (4). A typical endo-perio lesion presents with apico-coronal involvement of the periodontium as observed both through clinical and radiologic examinations (4). Periodontal lesions are always present but must be distinguished separately; namely, periodontal lesions of endodontic origin and plaque-induced periodontal lesions must be categorised accurately. Due to their different aetiology and pathogenesis (4).
Periodontal lesions deriving from pulp infection are found at or near the root apex or may also originate laterally where infection drains via lateral canal foramina (4). Conversely, periodontitis caused by bacterial plaque (biofilm) at the periodontal margin is usually identified at a more coronal level of the root (4).
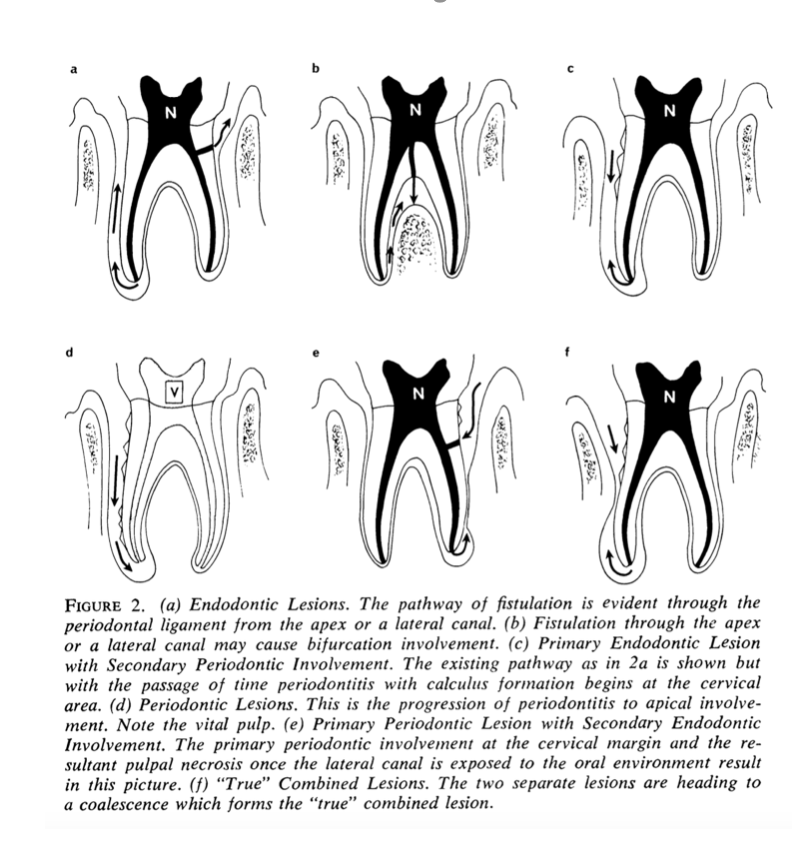
Fig. 1
Simon et al 1972 (8)
- Primary Endodontic Lesions
- Primary Endodontic Lesions With Secondary Periodontic Involvement
- Primary Periodontic Lesions
- Primary Periodontic Lesions With Secondary Endodontic Involvement
- "True" Combined Lesions
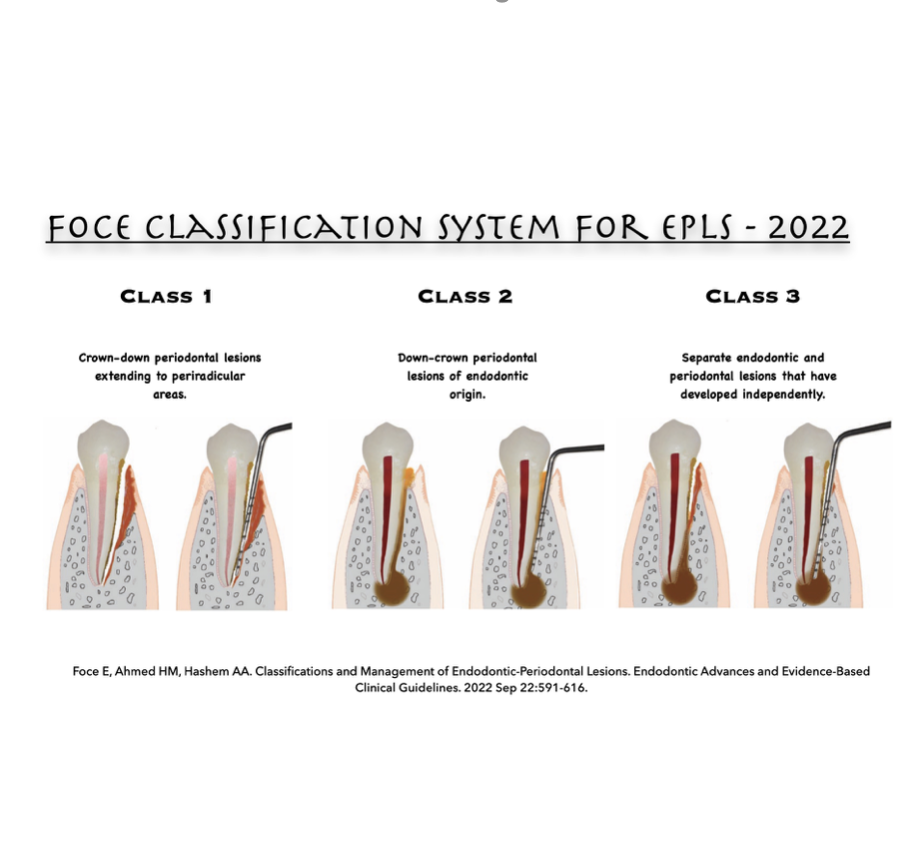
Fig. 2
Foce Classification System for EPLs - 2022 (9)
Class 1 – Crown-down Plaque-induced Periodontal Lesions
- Start from the crown and propagate along the root apically to deep periradicular areas.
- May lead to signs and symptoms mimicking pulp disease, with no pulp involvement
- It requires only periodontal treatment or at a later stage it may involve the pulp tissues through lateral canals or the apical foramen that requires root canal treatment followed by periodontal treatment.
Class 2 – Down-crown Periodontal Lesions of Endodontic Origin
- Start from the apical foramen or patent accessory canals in an apico-coronal direction. Through the periodontal ligament.
- Can cause periodontitis but will not lead to irreversible loss of the periodontal tissue attachment unless left untreated.
Class 3 – Combined Endo-perio Lesions
- A plaque-generated pocket extending apically and merging with a periodontal lesion of endodontic origin that developed at the root apex.
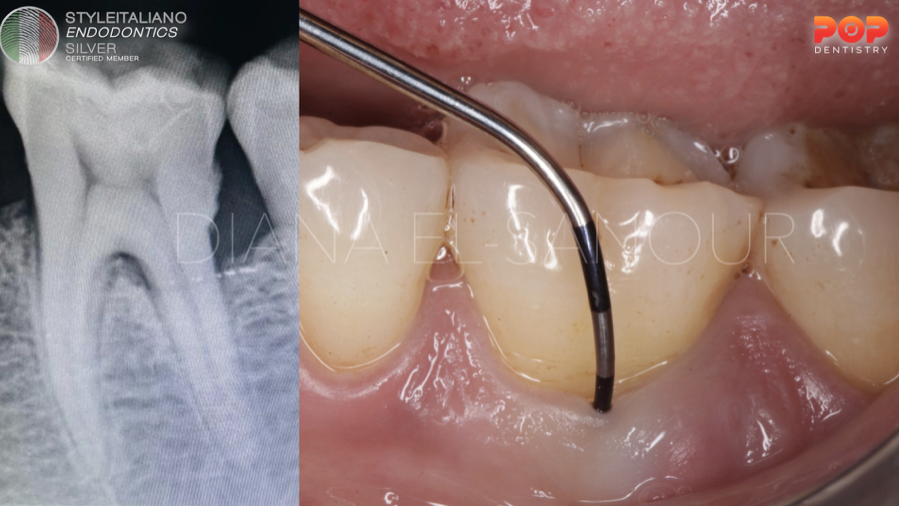
Fig. 3
Class 1 – Crown-down Plaque-induced Periodontal Lesions
periodontitis caused by bacterial plaque (biofilm) at the periodontal margin. it is identified at a more coronal level of the root.
A clinical case of 45 female patient presented with pain related to the lower 1st molar on the left side. Upon radiographic examination, it was presented with crystal bone loss related to the distal root with presence of evident local factors beyond the CEJ. While clinically it was presented with grade II furcation involvement (Glickman’s classification) only on the buccal side. treatment was initiated 1st non surgically with phase I therapy and surgical treatment after two weeks with open debridement.
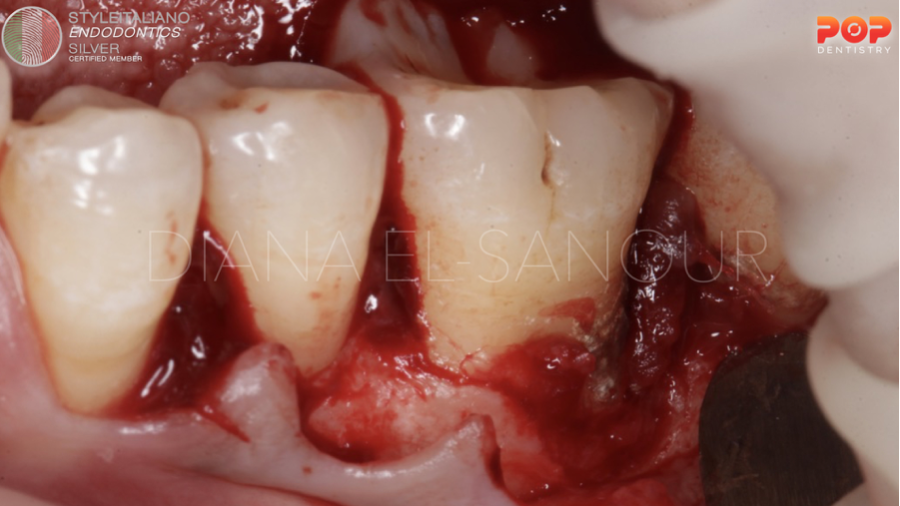
Fig. 4
Large amount of local factors related to the furcation area and the distal root.

Fig. 5
Open debridement.

Fig. 6
Suturing

Fig. 7
Class 2 – Down-crown Periodontal Lesions of Endodontic Origin
pulpal infection deriving from pulp and propagating coronally along the root. It is found at/near the root apex or laterally through lateral canals.
A 49 year old female patient presented clinically with broken old amalgam restoration related to the lower 2nd molar on the left side.
Upon clinical examination, it a fistulous tract through the gingival margin with probing depth of 7mm mid buccal point, 5mm mesially.
Upon radiographic examination, it has periapical radiolucency related to the medial tooth. And large amalgam restoration coronally with amalgam pin near the distal pulp horn.
Treatment was initiated endodontically and post-endodontic restoration.
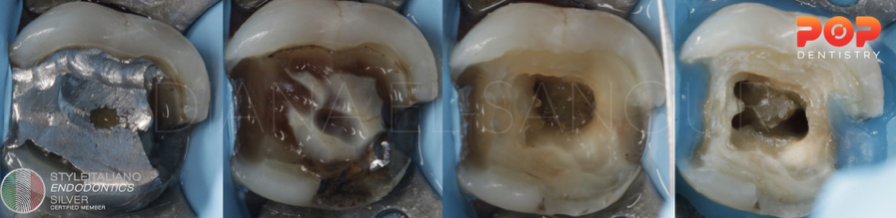
Fig. 8
Isolation and Access cavity Preparation.
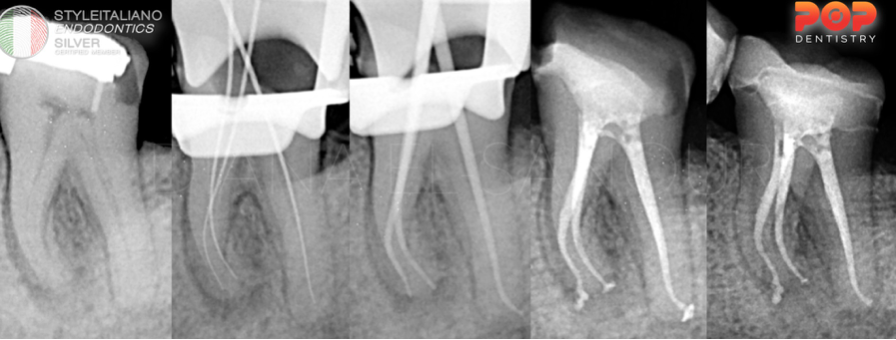
Fig. 9
Radiographic sequence of root canal treatment.
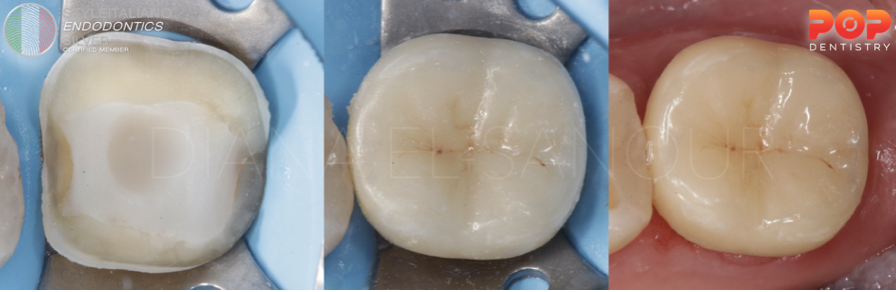
Fig. 10
Post Endodontics restoration; Preparation and cementation of an overlay.

Fig. 11
One month follow up; 2 mm PD buccal and 2 mm PD mesially.
Complete Healing of EPL.

Fig. 12
Class 3 – Combined Endo-perio Lesions
A plaque-generated pocket extending apically and merging with a periodontal lesion of endodontic origin that developed at the root apex.
The pulpal disease is limited only to the root canal space and does not involve the periradicular tissues either radiographically (no widening in the PDL space) or clinically (no pain on palpation or percussion). It’s noted in patients with generalized marginal periodontitis.
A 40 female old patient presented with continuous pain related to the lower 1st molar on the right side. Clinical examination revealed class V decay on the mesial line angle buccally. Deep periodontal pocket mesially with deep PD of 6 mm. and Class I miller Classification of recession. Radiographic examination revealed large class II amalgam restoration that is very close to the pulp on the distal side and large angular bone loss related to the mesial root.
Treatment was done for both pulp and periodontal tissue.
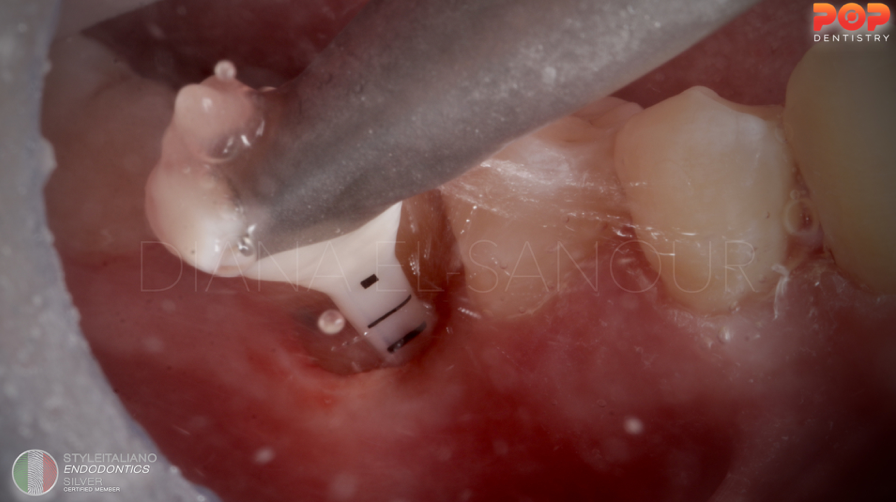
Fig. 13
Phase I therapy first with EMS airflow for removal of local factors.
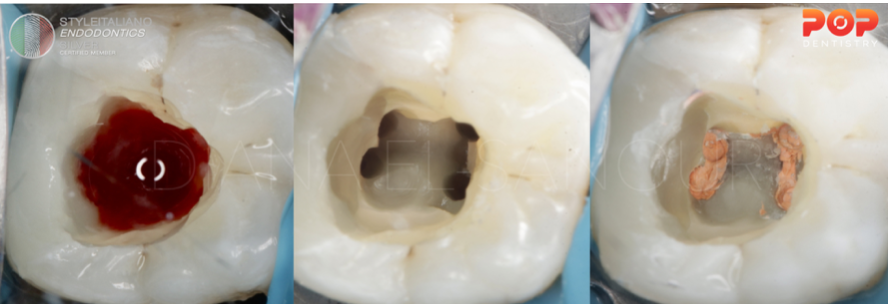
Fig. 14
Endodontic treatment; Amalgam removal, pre-endo build up and access cavity preparation.

Fig. 15
Post Endodontic filling and restoration of the class V cavity.

Fig. 16
Periodontal treatment; Minimally invasive technique.
One vertical incision preserving the interdental papillae.
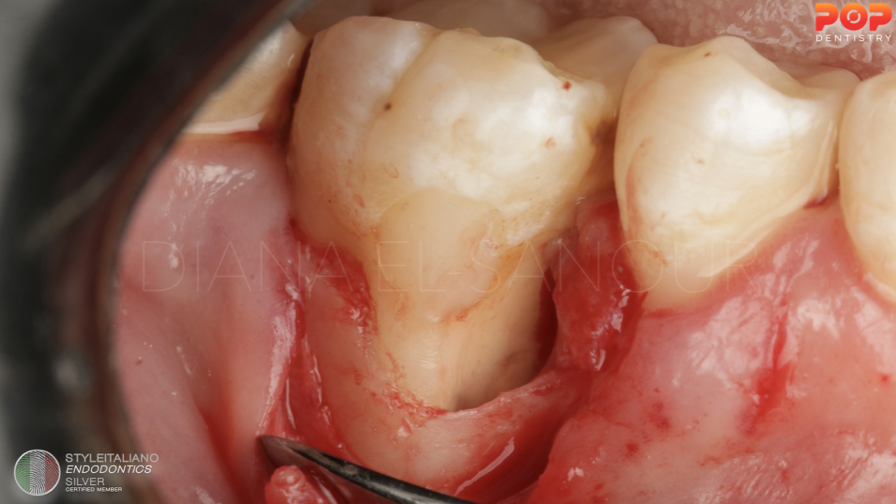
Fig. 17
Flap reflection; 3 osseous walled defect.

Fig. 18
Connective tissue graft harvesting from the palate.

Fig. 19
CTG suturing with 7-0 prolene suture.
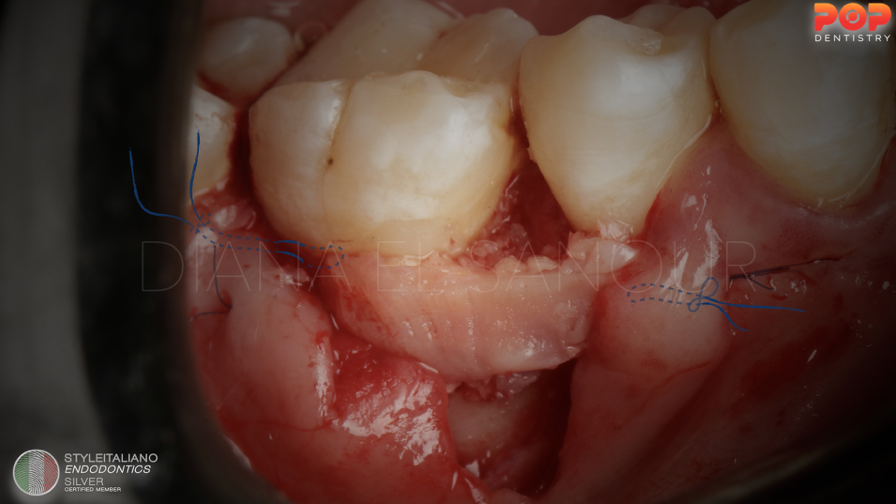
Fig. 20
Alloplast Bone grafting.
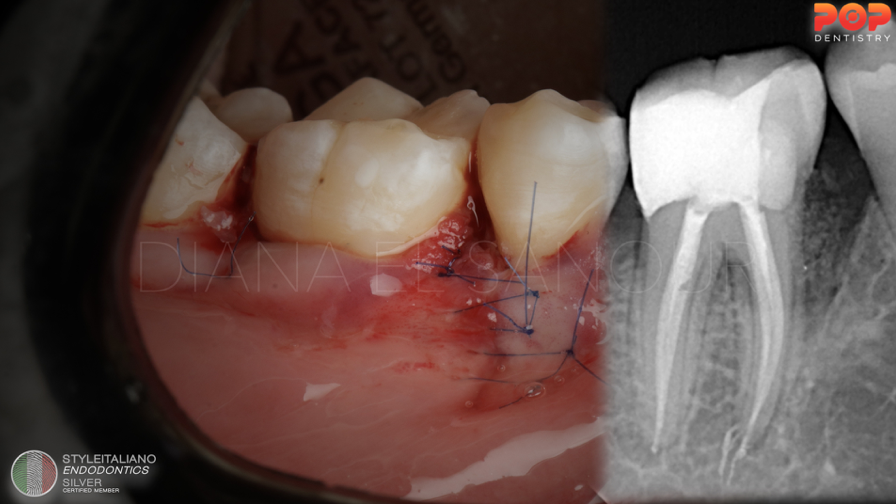
Fig. 21
Suturing and post operative radiograph
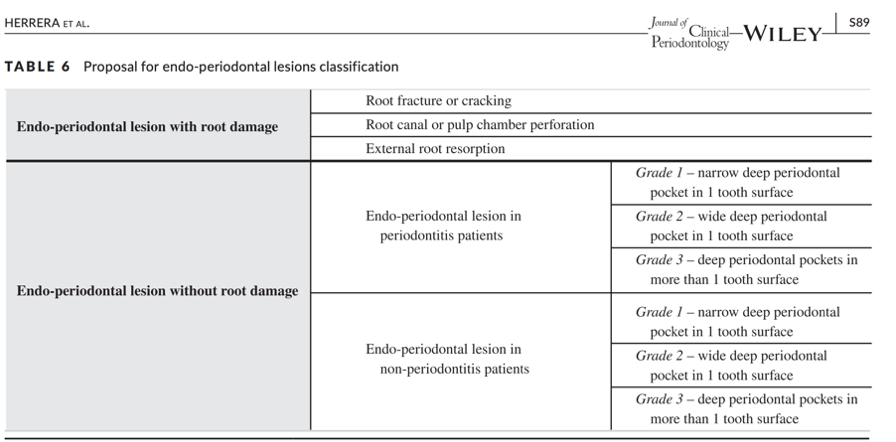
Fig. 22
Herrera et al. proposed a new classification of EPLs into those without root damage or with root damage.
EPLs without root damage primarily arise from bacterial infections in pulp and/or periodontal tissues.
EPLs with root damage arise from vertical tooth defect, perforation defect, or resorptive defects.
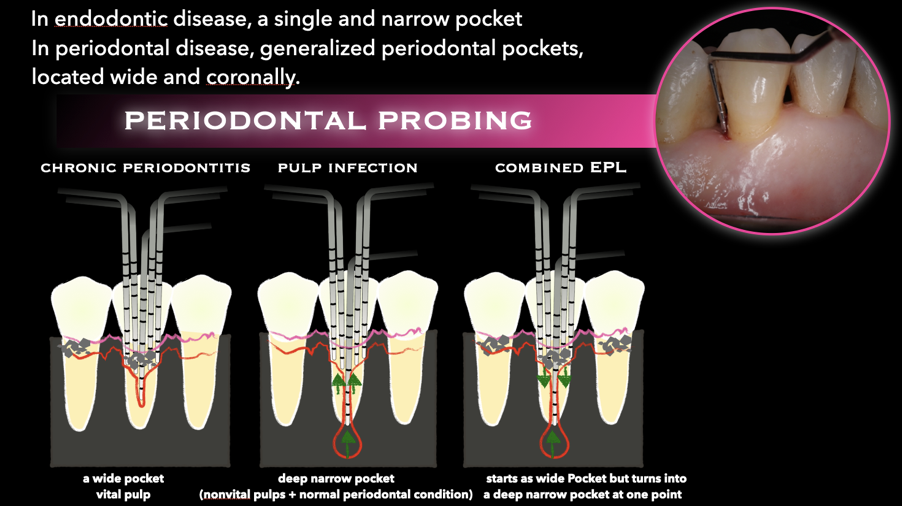
Fig. 23
Diagnosis of EPLs (11)
- Radiographic Evaluation;
In endodontic disease, bone loss is localized and mostly in the apical area.
In periodontal disease, bone resorption is more generalized and mostly at the crestal bone. - Pulp testing;
In endodontic disease, the tooth is non-vital.
In periodontal disease, the tooth is vital in most cases. - Palpation and percussion;
- Applying firm digital pressure to the mucosa covering the roots and apices.This will detect the presence of periradicular abnormalities or ‘‘hot’’ zones that produce painful response.
- An abnormal positive Percussion response indicated inflammation of the PDL that may be either from pulpal or periodontal origin. - Clinical signs; sinus or fistulas tract.
- Tooth Mobility; Hypermobility is quite common in cases of primary endodontic involvement and should not be confused with true mobility caused by periodontal destruction.
- Periodontal probing
Conclusions
Management of endo-perio lesions (EPLs)
- All endo-perio lesions should be diagnosed first before considering the treatment plan.
- When primary disease of one tissue, i.e. pulp or periodontium, is present and secondary disease is just starting, treat the primary disease. When secondary disease is established and chronic, both primary and secondary diseases must be treated.
- Wndodontic therapy precedes periodontal therapy.
- Periodontal therapy may or may not be required, depending on disease status.
- The complete healing of destroyed periodontal support can be expected following the Endodontic treatment .
- The resolution of extensive destruction following the treatment of chronic periodontitis is less predictable. periodontal therapy, including deep scaling with and without periodontal surgery, should be postponed until the result of the endodontic treatment can be evaluated.Management of endo-perio lesions (EPLs)
Bibliography
- Newman MG, Facd D, Klokkevold PR, Dds MS, Elangovan S, Dmsc BD, Kapila Y. Newman and Carranza's Clinical Periodontology and Implantology E-Book. Elsevier Health Sciences; 2023 Jun 5.
- Kirkham DB. The location and incidence of accessory pulpal canals in periodontal pockets. J Am Dent Assoc. 1975;91(2):353–356 (1939).
- Giuliana G, Ammatuna P, Pizzo G, et al. Occurrence of invading bacteria in radicular dentin of periodontally diseased teeth: microbiological findings. J Clin Periodontol. 1997;24(7):478–485.
- Schäfer E. Endodontic advances and evidence-based clinical guidelines. European Endodontic Journal. 2023;8(3):237.
- Peeran SW, Thiruneervannan M, Abdalla KA, Mugrabi MH. Endo-perio lesions. Int J Sci Technol Res. 2013 May;2(5):268-74.
- Abbott, P.V. and Salgado, J.C. (2009). Strategies for the endodontic management of concurrent endodontic and periodontal diseases. Aust Dent J 54 (Suppl 1): S70–S85.
- Ahmed, H.M.A. (2012). Different perspectives in understanding the pulp and periodontal intercommunications with a new proposed classification for endo-perio lesions. ENDO
– Endod Pract Today 6 (2): 87–104. - Simon JH, Glick DH, Frank AL. The relationship of endodontic‐periodontic lesions. Journal of periodontology. 1972 Apr;43(4):202-8.
- Foce E, Ahmed HM, Hashem AA. Classifications and Management of Endodontic‐Periodontal Lesions. Endodontic Advances and Evidence‐Based Clinical Guidelines. 2022 Sep 22:591-616.
- Herrera, D., Retamal-Valdes, B., Alonso, B., and Feres, M. (2018). Acute periodontal lesions (periodontal abscesses and necrotizing periodontal diseases) and endo-periodontal lesions. J Clin Periodontol 45 (Suppl 20): S78–S94.
- Shenoy N, Shenoy A. Endo-perio lesions: Diagnosis and clinical considerations. Indian Journal of Dental Research. 2010 Oct 1;21(4):579-85.



