Dental Trauma: Forever classic, Never boring
06/06/2024
Fellow
Warning: Undefined variable $post in /home/styleendo/htdocs/styleitaliano-endodontics.org/wp-content/plugins/oxygen/component-framework/components/classes/code-block.class.php(133) : eval()'d code on line 2
Warning: Attempt to read property "ID" on null in /home/styleendo/htdocs/styleitaliano-endodontics.org/wp-content/plugins/oxygen/component-framework/components/classes/code-block.class.php(133) : eval()'d code on line 2
A 23 years old, female patient, was referred to my practice for an endodontic treatment on tooth 11. Patient complained of pain above the root and was concerned of the discoloration.
Patient reported previous trauma (15 years ago) and an attempted endodontic treatment (5 years ago).
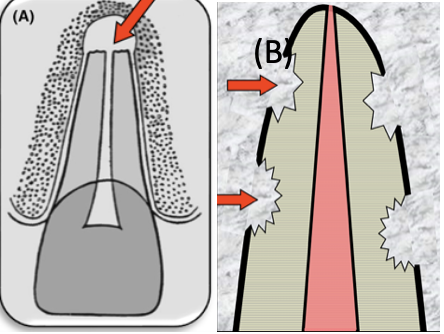
Fig. 1
Traumatic dental injuries constitute one of the main reasons for the need of endodontic treatment, ranging from 17-29%. This is due to the development of cracks, fractures and/or dentinal exposure that permits bacterial penetration to the pulp. In severe cases (avulsion, intrusion, luxation), damage to vessels at the apical foramen can lead to necrosis. One of the most destructive manifestations after trauma is the root resorption. The resorption can be internal or external based on the location, whereas, based on the characteristics and cause of the lesion, can be classified as inflammatory, replacement, surface, invasive and pressure. The main pre-requirement for the initiation of resorption is the damage of outer protective layers (pre-dentine, pre-cementum) and/or PDL. This damage will activate clastic cells which will resorb hard tissues (tooth and bone). If the pulp and root canal were infiltrated ,or become infiltrated at later stage, by bacteria then the resorption will progress as inflammatory (A). In the absence of bacteria, the damage at the protective layers and PDL will activate clastic cells from the surrounding bone, which will be followed by osteoblastic cells forming bone at the area of resorption (B). Sometimes, the invading tissue is fibrous connective tissue which later presents ectopic calcifications giving a mixed radiolucent-radiopaque image.
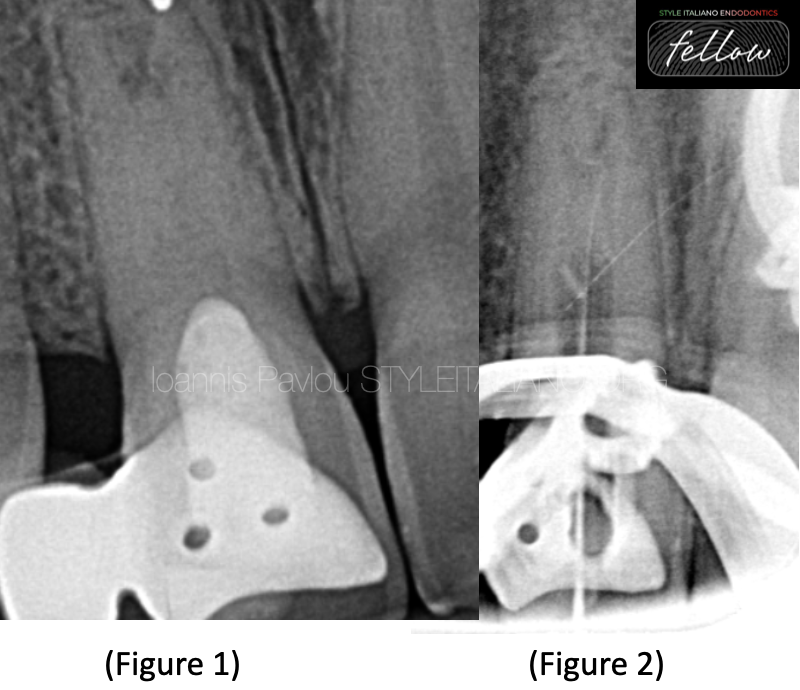
Fig. 2
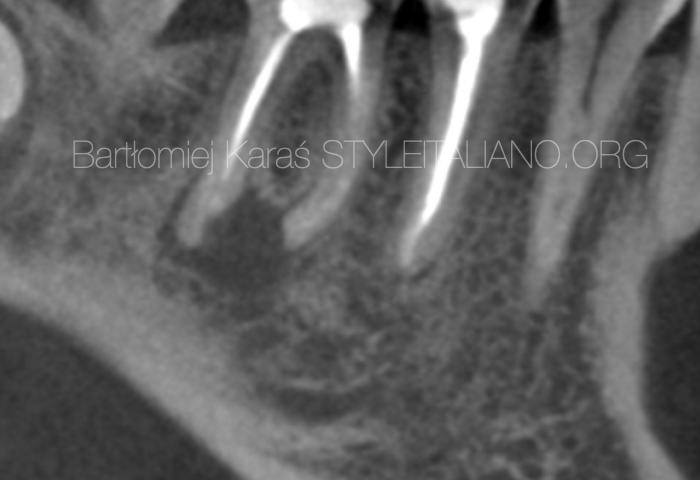
Figure 1 shows preoperative x-ray of tooth 11. The tooth is the abutment of a Richmond bridge with pontic being tooth 12. The pulp chamber is filled with material (Zinc oxide) up to CEJ. The root canal space is obliterated at the cervical and mid portions of the root, while in the apical part seems to have calcifications and an open apex.
After anaesthesia and isolation, the pulp chamber was opened and the restorative material was removed. With the aid of delicate ultrasonic tips, the calcifications were troughened and removed until a narrow canal entrance was identified.
Using small hand files C-pilot and D-finder, under copious irrigation of EDTA, a no 6 K-file managed to reach the apex, which was verified with Apex locator and an interim x-ray (fig.2).
The interim x-ray revealed a strange route of the root canal as also the impression of two possible root apices. For that reason it was decided to proceed to chemomechanical disinfection of the existing canal using rotary files of small taper ( 3-4%), placement of intracanal medicament (CaOH2) and referral for CBCT.
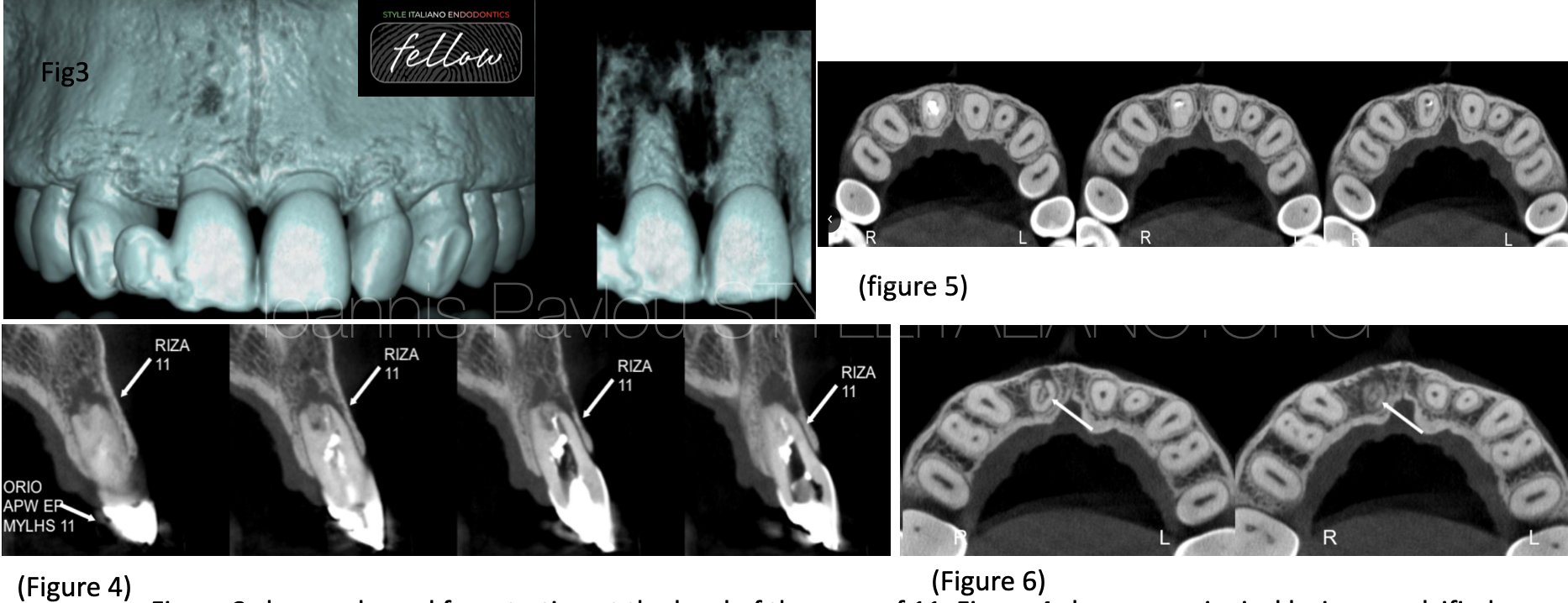
Fig. 3
Figure 3 shows a buccal fenestration at the level of the apex of 11. Figure 4 shows a periapical lesion, a calcified tissue within the resorption area and 2 portal exits, one in middle of the root apex and one exiting buccally. These findings were also verified in the coronal slides, where was also identified a radiolucent circumferential line surrounding the calcified tissue (fig 6). The main canal presents a direction from mid-buccal to mesial-palatal (fig 5-6). The periapical lesion, the existence of calcified tissue and the invasion of this tissue in the root canal space, might show a combination of resorption types.

Fig. 4
Based on the aforementioned findings, the chemomechanical disinfection was completed up to 40.04 with copious irrigation of NaOCl 5.25%, EDTA 17% with the aid of ultrasonic activation. This time it was decided to place as intracanal medicament for two weeks Ledermix, a corticosteroid-antibiotic paste.The two main active components CS-AB paste can reduce inflammation, inhibit clastic cells and kill bacteria.

Fig. 5
Two weeks later, the patient returned to the practice free of symptoms. After anaesthesia and isolation, a full cycle of irrigation under ultrasonic activation was done. The root canal was dried with intracanal suction and paper points. A cone fit x-ray was taken. The gutta-percha point was slightly extruded so it was decided to use a larger size (45.04).

Fig. 6
For the obturation, it was decided to proceed with WVC and bioceramic sealer (Avalon Neosealer). An MTA plug could have been used too, but because the root canal was not straight , it would not be easy to direct the material towards all ramifications. Therefore, the root canal system was filled with bioceramic sealer and the cone was used as a plugger in order to push the sealer everywhere. The cone was placed, cut and downpacked to fill the remaining gaps. The patient was returned back to the referral dentist, to fill the remaining part of the canal with flowable resin, do a permanent restoration and after the recall and justification of healing, to continue with a new prosthetic solution.

Fig. 7
About the author:
I graduated as a Certified Dental technician in 1995 from the Technological Educational Institution of Athens. In 2002 I completed my dental studies at the Aristotle University of Thessaloniki. I worked and studied in the UK for 8 years completing a series of postgraduate studies, the most important being the Postgraduate Diploma in Endodontics (Queen Mary, London) and the Postgraduate Diploma in Periodontology (University of Central Lancashire). I returned to Greece in 2010 and since 2015 I have been the principal of a clinic limited in Endodontics and Periodontics. In 2022 I completed the MSc in Prosthodontics at the University of Siena with a special interest in bruxism and TMD.
Conclusions
Traumatic dental injuries can present several problems to teeth, from dentinal cracks and fractures to necrosis and root resorption. Especially the latter, can take the form of many types such are external inflammatory, replacement or invasive. Dentists should be able to identify the type and decide for the most appropriate approach to disinfect the root canal system, arrest the resorptive process and seal the root canal especially at the apex which due to the resorption can be irregular and wide.
Bibliography
- Krastl, Gabriel & Weiger, Roland & Filippi, Andreas & Waes, H. & Ebeleseder, Kurt & Ree, Marga & Connert, Thomas & Widbiller, Matthias & Tjäderhane, L. & Dummer, Paul & Galler, K.. (2021). Endodontic management of traumatized permanent teeth – a comprehensive review. International Endodontic Journal. 54. 10.1111/iej.13508.
- Rosa Scavo, Ricardo Martinez Lalis, Osvaldo Zmener, Sandra DiPietro, Daniel Grana, Cornelis H. Pameijer. (2011). Frequency and distribution of teeth requiring endodontic therapy in an Argentine population attending a specialty clinic in endodontics, International Dental Journal, Volume 61, Issue 5, Pages 257-260, ISSN 0020-6539, https://doi.org/10.1111/j.1875-595X.2011.00069.x.
- Abbott PV, Lin S. Tooth resorption— Part 2: A clinical classification. Dental Traumatology. 2022;38:267–285. https://doi.org/10.1111/edt.12762
- Bryson EC, Levin L, Banchs F, Abbott PV, Trope M. Effect of immediate intracanal placement of Ledermix Paste on healing of replanted dog teeth after extended dry times. Dent Traumatol. 2002;18:316–21.
- Pierce A, Heithersay G, Lindskog S. Evidence for direct inhibition of dentinoclasts by a corticosteroid/antibiotic paste. Endod Dent Traumatol 1998; 4: 44–45.
- Cvek M, Abbott PV, Bakland LK, Heithersay GS. Management of trauma related pulp disease and tooth resorption. In: JO Andreasen, FM Andersson, L Andersson, editors. Textbook and color atlas of traumatic injuries to the teeth. 5th ed. Copenhagen: Wiley; 2019. p. 648–717.
- Clinical Outcome of Non-Surgical Root Canal Treatment Using a Single-cone Technique with Endosequence Bioceramic Sealer: A Retrospective Analysis, Chybowski, Elizabeth A. et al. Journal of Endodontics, Volume 44, Issue 6, 941 - 945