
Danger zone in C-shaped root canals
28/05/2023
Fellow
Warning: Undefined variable $post in /var/www/vhosts/styleitaliano-endodontics.org/endodontics.styleitaliano.org/wp-content/plugins/oxygen/component-framework/components/classes/code-block.class.php(133) : eval()'d code on line 2
Warning: Attempt to read property "ID" on null in /var/www/vhosts/styleitaliano-endodontics.org/endodontics.styleitaliano.org/wp-content/plugins/oxygen/component-framework/components/classes/code-block.class.php(133) : eval()'d code on line 2
The danger zone is an area of the root canal where the primary thickness of dentin before preparation is under 1 mm. In general, the danger zone is located 4 to 6 mm below the canal chamber orifice. A danger zone can appear in the buccal root of maxillary premolars and molars and in the distal area of the mesial root and mesial region of the distal root of the mandibular molars. The cause of forming C-shaped canals and the prevalence of the danger zone in C-shaped roots is a failure of Hertwig's epithelial root sheath to fuse on the lingual or buccal root surface. If Hertwig's epithelial root sheath fails to fuse on the lingual surface, then the groove and danger zone occur on the lingual side of the root. If the root sheath fails to unite on the buccal surface-danger zone appears on the buccal side. There is almost always a danger zone in roots containing C-shaped root canals. Very little dentin separates the external surface from C-shaped canal system, thereby increasing the possibility of perforation during endodontic treatment and prosthetic restoration. (Melton et.al. JOE 1991). In 80% of C-shaped root canals in mandibular molars, invagination and correlated danger zone occurs in 80% lingually, 19% buccally, and only 1% have no groove or danger zone (Avi Shemesh, Avi Levin, Vered Katzenell, Joe Ben Itzhak, Oleg Levinson, Zini Avraham, Michael Solomonov. Clinical Oral Investigations 2017). Lingual walls in C-shaped roots are usually thinner than buccal walls at the coronal, middle, and apical third of the roots, especially at the mesial locations, compared to the danger zone in standard lower molars, which is situated 4-6 mm below the canal orifices. The lowest value of dentine thickness in C-shaped root canals was 0,26 mm (Wen Lin Chai and Yo Len Thong JOE 2004). The danger zone in the mandibular premolars with C-shaped roots was situated lingually, mesially, or mesiolingually (.Avi Shemesh, DMD, Ella Lalum, DMD, Joe Ben Itzhak, DMD, Dan Henry Levy, DMD, MSc, Alex Lvovsky, DMD,Oleg Levinson, DMD, and Michael Solomonov, DMD JOE 2020). That's why we need to plan treatment and instrumentation according to the location of DZ. In the case of the position of invagination at the lingual side, we need to avoid lingually sweeping movements. If the invagination is situated buccally, we avoid sweeping motions on the buccal side. Due to the high risk of strip perforation, it is recommended to work with instruments of small taper 02, 04, 00, for example, XP-finisher or regressed taper such DC-taper 2 H SS-white, TrueNatomy Dentsply Sirona. Knowledge of anatomy is necessary to perform successful root canal treatment. Lack of awareness about the presence, location, and value of danger zone due to incomplete diagnostic can lead to over-instrumentation and failure, such as strip perforation and vertical root fracture. Incredibly challenging are re-treatment and broken file removal cases in C-shaped root canals because of the previous preparation of the danger zone. It finds no literature about the re-treatment or broken file removal in C-shaped root canals, but cases exist. In separated file cases, bypass is preferable. In prosthetic reconstruction, custom posts are not recommended due to the high risk of perforation during preparation.

Fig. 1
50-year-old patient was referred to me with information about suspicion of separation of 2 instruments while performing a root canal treatment. On clinical examination, temporary filling IRM was detected. No signs of crack or fracture. The probing depth was no more than 3 mm. No pain on percussion or palpation. Pulp status: Necrosis. Diagnosis: Asymptomatic apical periodontitis. Pre-opp CBCT examination, the axial slice showed a C-shaped root canal type C2, according to Melton and Fan. It was noticed the presence of a danger zone in a lingual groove. The lowest value of dentin thickness according to measurement was under 0,5 mm.

Fig. 2
Pre-opp examination CBCT, sagittal slice showed the presence of a separated instrument in apical part of ML root canal and a separated instrument in the coronal part of MB root canal. A periapical lesion was present. Because of the lingual location of the danger zone and a low value of dentin sickness, I made a decision to perform a bypass in ML root canal. An instrument from the coronal part of MB root canal was successfully removed by using the ultrasonic removal technique.

Fig. 3
Intra-op X-ray showed performed bypass in ML root canal and achieved working length in MB and D root canals. Bypass was performed by using hand files (C-pilot) from ISO 08 to 20 and machine files DC-taper 2H SS-white. ML, MB, and D root canals were instrumented to ISO 30.06 by DC-taper 2H SS-white. Endodontic solutions were activated by EDDY VDW and XP-endo finisher FKG Dentaire.
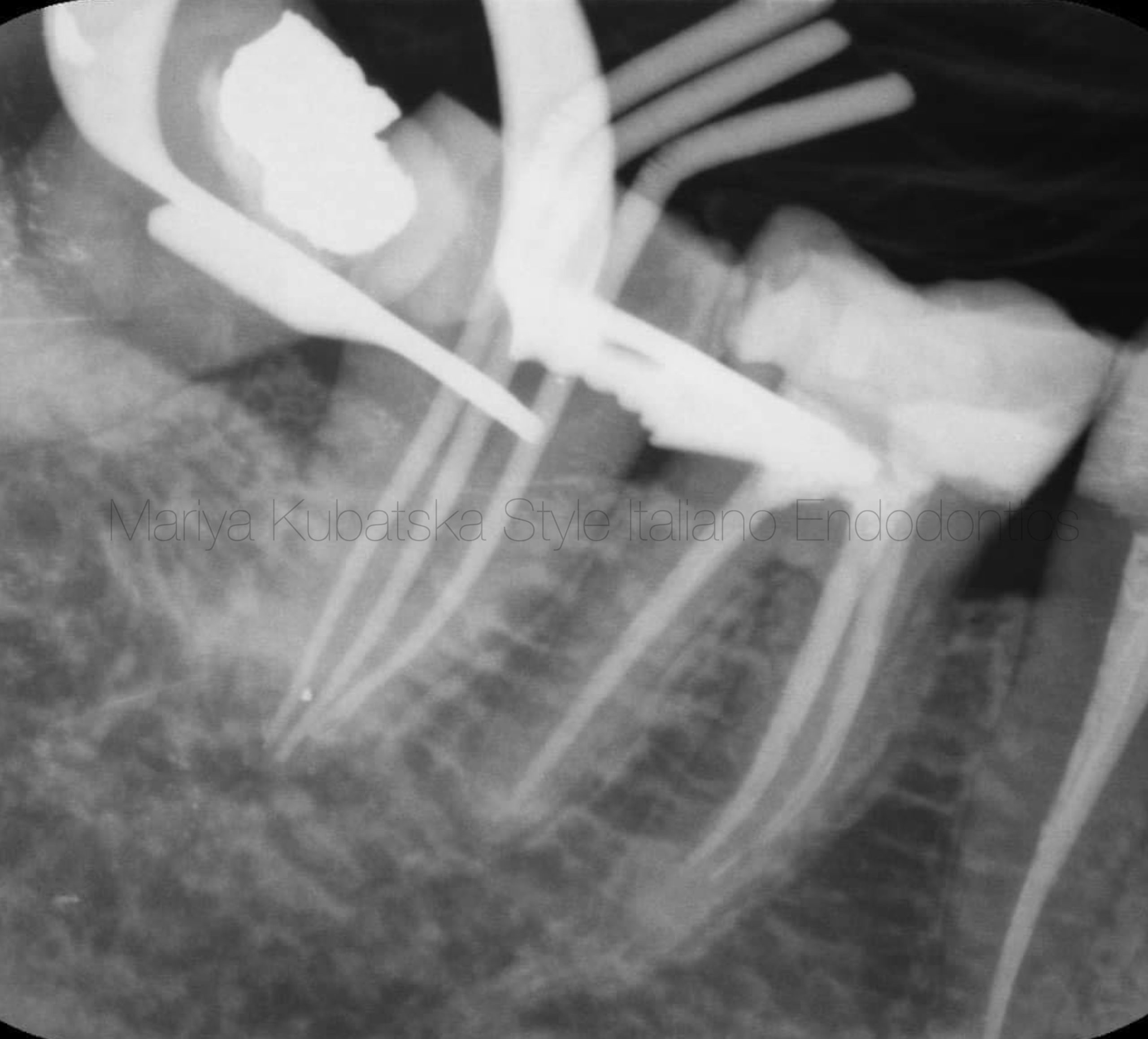
Fig. 4
Intra-op X-ray with gutta-percha points showed correct working length in all root canals.

Fig. 5
The appearance of the pulp chamber after the phases of shaping and cleaning.

Fig. 6
Post operative x-ray. Obturation was made with epoxy sealer and gutta-percha by using hybrid technique. The hybrid technique is a combination of lateral and vertical compaction. The apical part of the canal is filled using the lateral compaction method, the remaining part using the vertical compaction method.
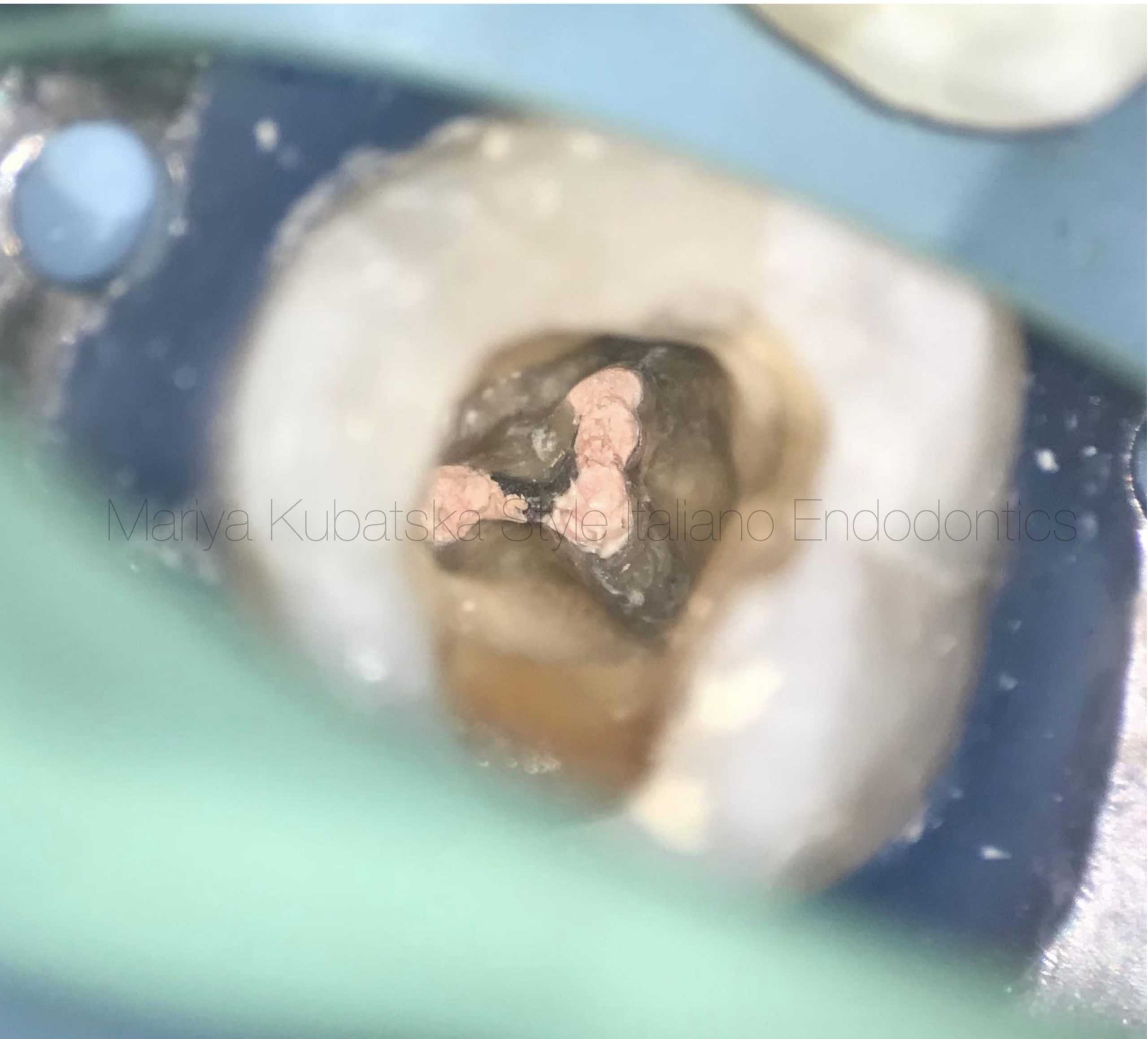
Fig. 7
The appearance of the pulp chamber after root canals obturation.
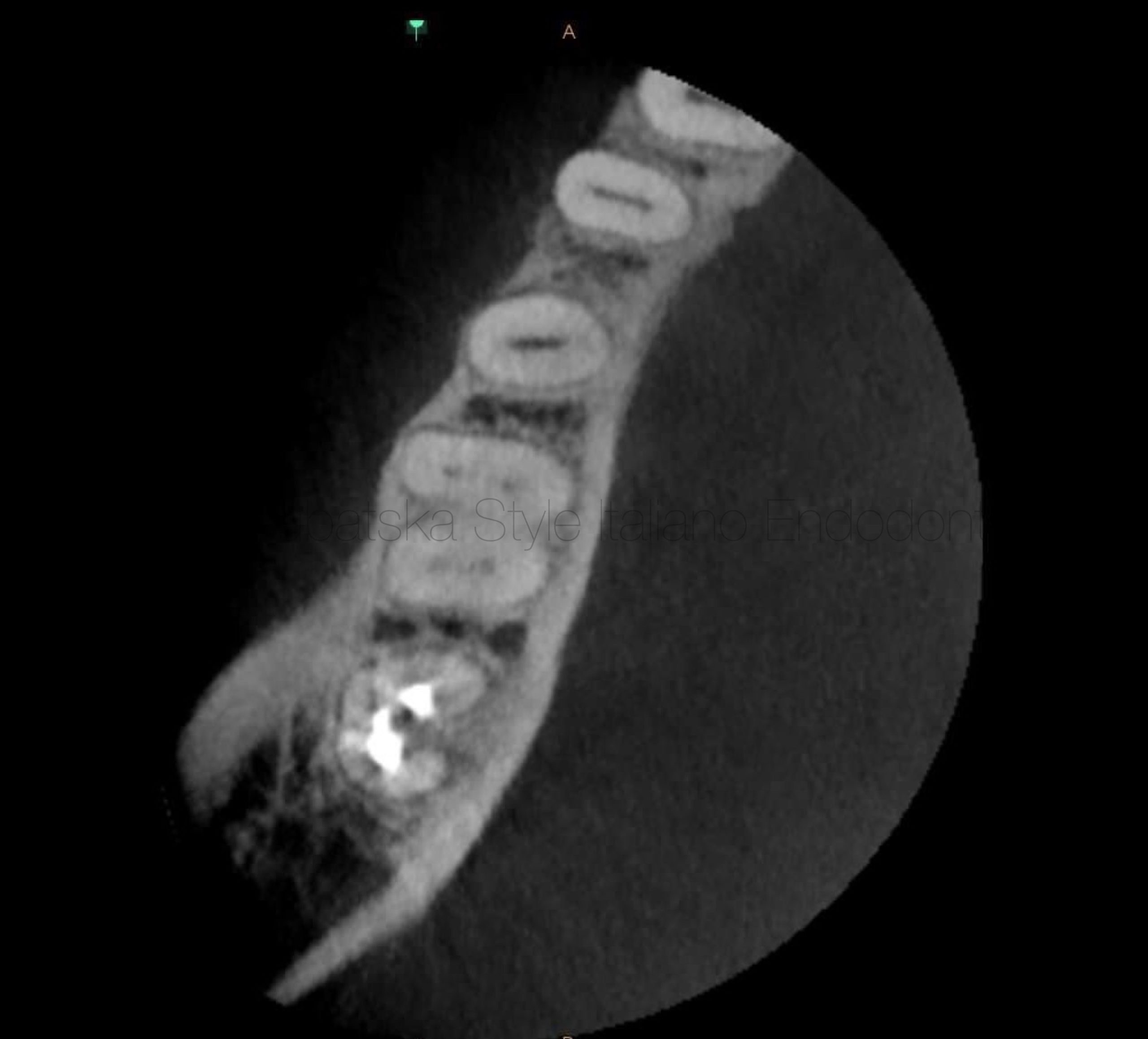
Fig. 8
A 40-year-old patient was referred to me for non surgical re-treatment of tooth 47. On clinical examination MOD composite filling was detected. No signs of crack or fracture. The probing depth was no more than 3 mm. No pain on percussion or palpation. Diagnosis and pulp status: Previously treated , asymptomatic apical periodontitis. Pre-opp CBCT examination, the axial slice showed a C-shaped root canal type C2, according to Melton and Fan. It was noticed the presence of a danger zone in a lingual groove. The lowest value of dentin thickness according to measurement was under 0,3 mm. It was suspicion of strip perforation during previous treatment.
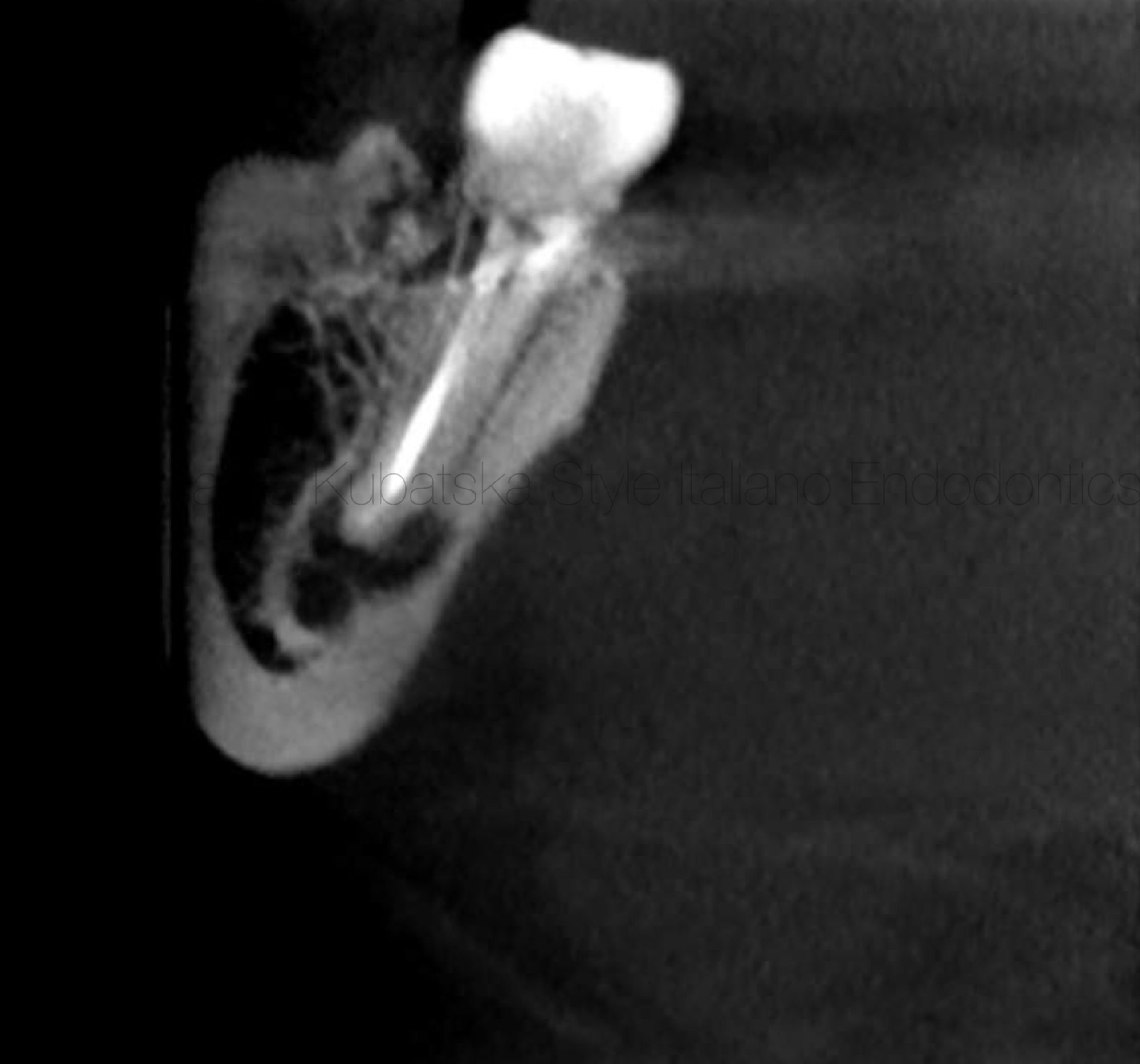
Fig. 9
Pre-opp examination CBCT, sagittal slice showed the presence of periapical lesion. The root of tooth 47 was found to be very close to the inferior alveolar nerve, what could cause complications during root canal treatment.

Fig. 10
The appearance of the pulp chamber after the phases of shaping and cleaning. Gutta-percha was removed mechanically using instruments Endostar Re Endo Rotary System, XP-endo shaper FKG Dentaire and Orange Guttane Cerkamed. ML, MB, and D root canals were instrumented to ISO 30.06 by DC-taper 2H SS-white. Due to its close location to the inferior alveolar nerve and high risk of complications was performed apical stop. Strip perforation wasn't detected, which was suspected earlier. Endodontic solutions were activated by EDDY VDW, XP-endo finisher FKG Dentaire.

Fig. 11
Intra-op X-ray with gutta-percha points showed correct working length in all root canals.

Fig. 12
Photo of calibrated gutta-percha points in root canals. Calibration was made by calibration ruler Dentsply Sirona.
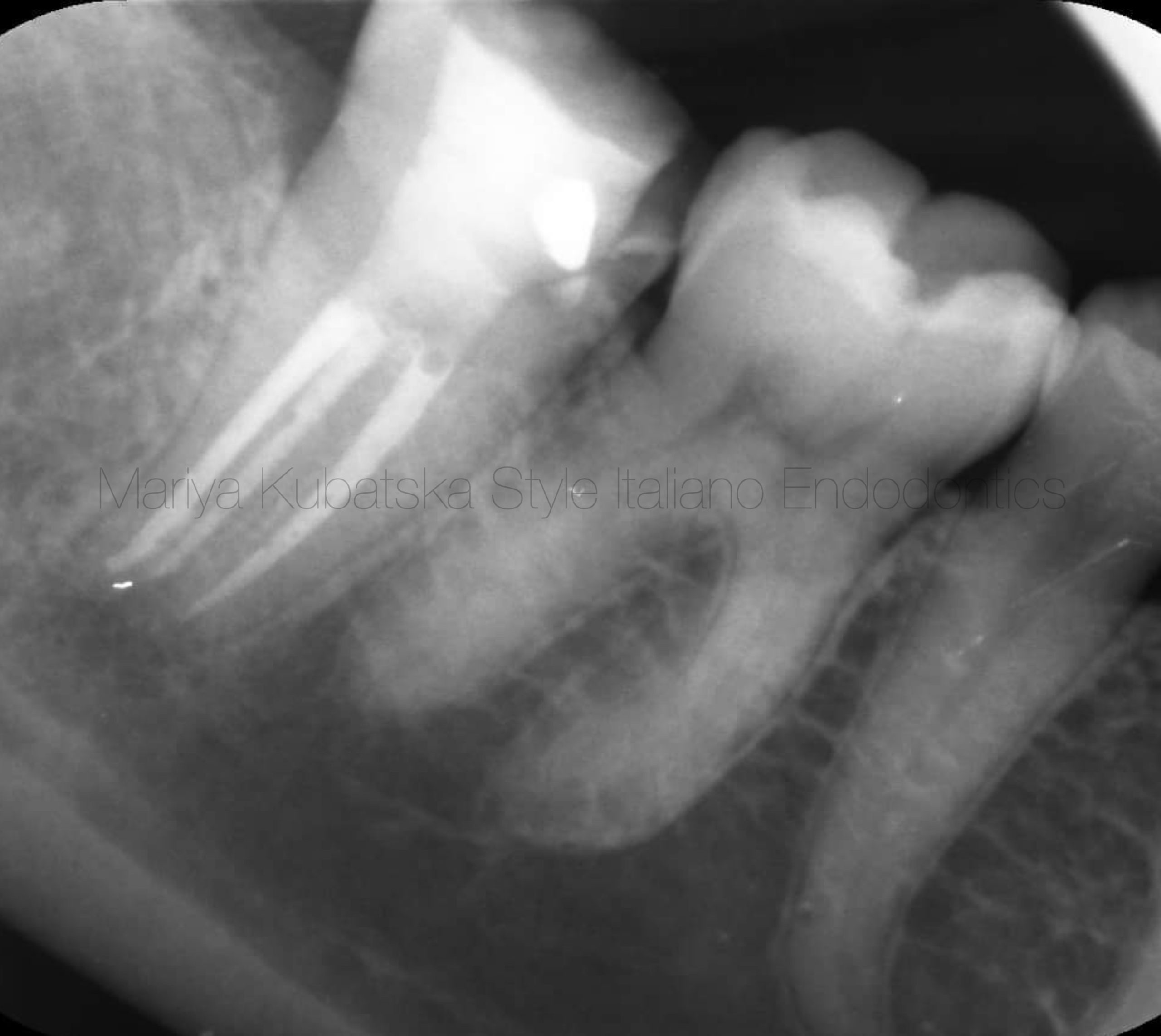
Fig. 13
Post operative x-ray. Obturation was made with epoxy sealer and gutta-percha by using hybrid technique.

Fig. 14
A view of the mesial and distal orifices after obturation.
Conclusions
C-shaped root canals can be very demanding for clinicians or operators due to complex anatomy and the appearance of danger zones. RCT of C-shaped root canals containing invaginations (grooves) can be challenging in every stage of treatment, from diagnosing, instrumentation, and obturation to post-endodontic restoration. That's why deep knowledge and awareness of anatomy are mandatory. Minimal invasive instrumentation is crucial to preserve dentin, which impacts tooth functionality and long-term prognosis.
Bibliography
1.C-shaped canals-prevalence and root canal configuration by cone beam computed tomography evaluation in first and second mandibular molars-a cross-sectional study.Avi Shemesh, Avi Levin, Vered Katzenell, Joe Ben Itzhak, Oleg Levinson, Zini Avraham, & Michael Solomonov .Clin Oral Investig 2017 Jul;21(6):2039-2044.doi: 10.1007/s00784-016-1993-y.Epub 2016 Nov 14.PMID: 27844150.
2.Cross-sectional Morphology and Minimum Canal Wall Widths in C-shaped Roots of Mandibular Molars.Wen Lin Chai, BDS, FDSRCS, and Yo Len Thong, BDS, MSc. JOE 2004.
3.Radicular Grooves and Complex Root Morphologies of Mandibular Premolars Among Israeli Population.
Avi Shemesh, DMD, Ella Lalum, DMD, Joe Ben Itzhak, DMD, Dan Henry Levy, DMD, MSc, Alex Lvovsky, DMD,Oleg Levinson, DMD, and Michael Solomonov, DMD.JOE 2020.
4.Anatomical and Histological Features of C-Shaped Canals in Mandibular Second Molars.Darlene C. Melton, DDS, Keith V. Krell, DDS, MS, MA, and Michel W. Fuller, DDS, MS.JOE 1991.
5.C-shaped Canal System in Mandibular Second Molars Part III: The Morphology of the Pulp Chamber Floor.Yi Min, DDS, MS, PhD,* Bing Fan, DDS, MS, PhD,* Gary S.P. Cheung, DDS, MDS,† James L. Gutmann, DDS, FACD, FICD,‡ and Mingwen Fan, DDS*JOE 2006.
6.C-shaped Canal System in Mandibular Second Molars Part IV: 3-D Morphological Analysis and Transverse Measurement.Yuan Gao, DDS, PhD,* Bing Fan, DDS, MDS, PhD,* Gary S. P. Cheung, DDS, MDS,† James L. Gutmann, DDS, FACD, FICD,‡ and Mingwen Fan, DDS*.JOE 2006.
7.Evaluation of a Rotary Instrumentation Method for C-shaped Canals with Micro-computed Tomography.Lisa H. M. Cheung, BDS, MDS, AdvDipEndodnt, and Gary S. P. Cheung, BDS, MDS, MSc, PhD.JOE 2008

