Perforation repair: step by step
25/03/2021
Zaher Al-taqi
Warning: Undefined variable $post in /home/styleendo/htdocs/styleitaliano-endodontics.org/wp-content/plugins/oxygen/component-framework/components/classes/code-block.class.php(133) : eval()'d code on line 2
Warning: Attempt to read property "ID" on null in /home/styleendo/htdocs/styleitaliano-endodontics.org/wp-content/plugins/oxygen/component-framework/components/classes/code-block.class.php(133) : eval()'d code on line 2
A tooth perforation is a pathologic or iatrogenic communication between the root canal space and the periodontal apparatus. To clinically determine if an endodontically perforated tooth should be extracted or saved, the clinician must first understand the prognosis and treatment. The biologic response of a perforated tooth is inflammatory and can cause a breakdown of the osseous and periradicular tissues. This can lead to a guarded long-term prognosis for the tooth. Much depends on the location, size, and time from occurrence. The more apical the perforation, the better the prognosis, but the more difficult the direct repair is. The larger the perforation, the more difficult sealing can be. The immediate sealing of a perforation is paramount to help prevent infection from communicating with the surrounding periradicular tissue.
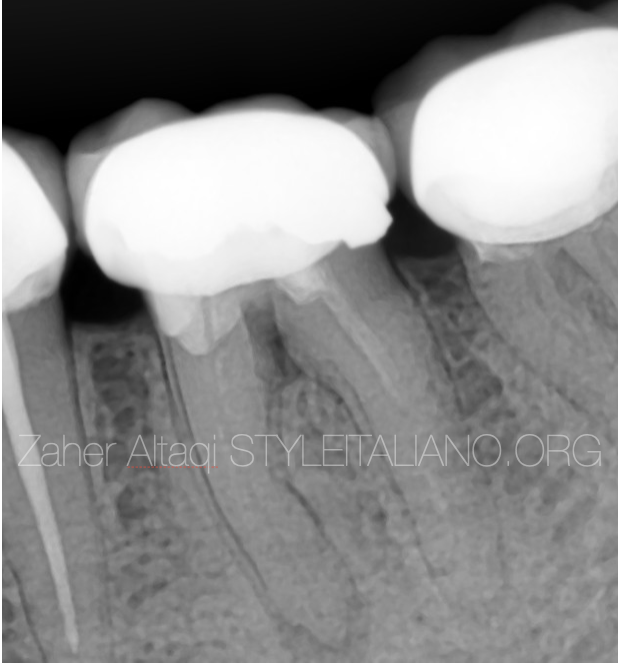
Fig. 1
40 years old patient presented to the clinic with moderate pain in the lower left area .
He described it on biting or chewing.
Upon clinical examination we found tenderness on percussion related to tooth 36.
Radigraphic examination revealed poor RCT and suspection of frucal perforation with furcal radiolucency .
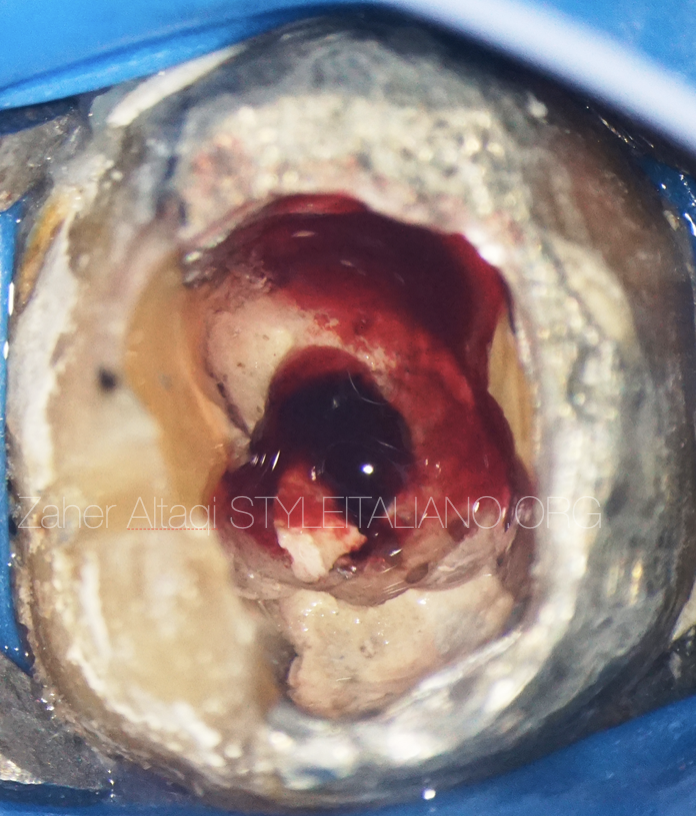
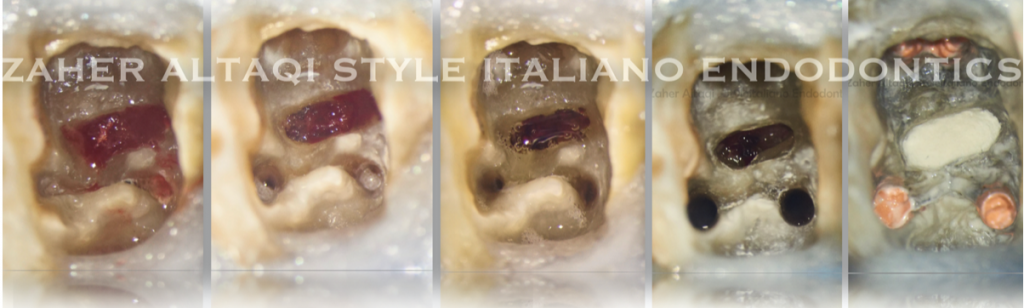
Fig. 2
Crown was removed, access was done through the old amalgam filling and base material. Severe bleeding was observed .
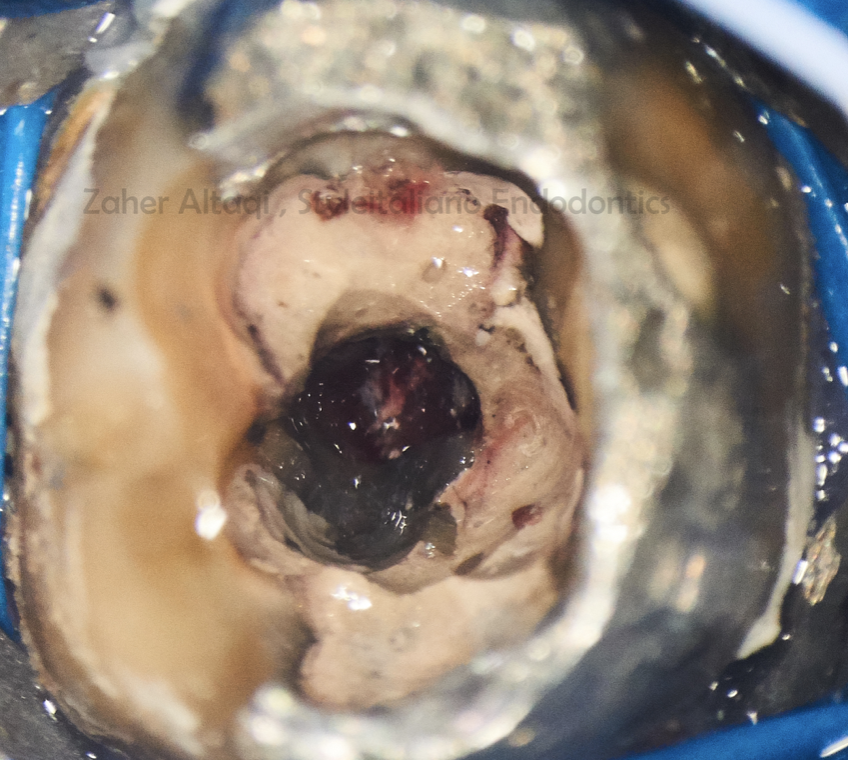
Fig. 3
After bleeding control, we can see the perforation site.
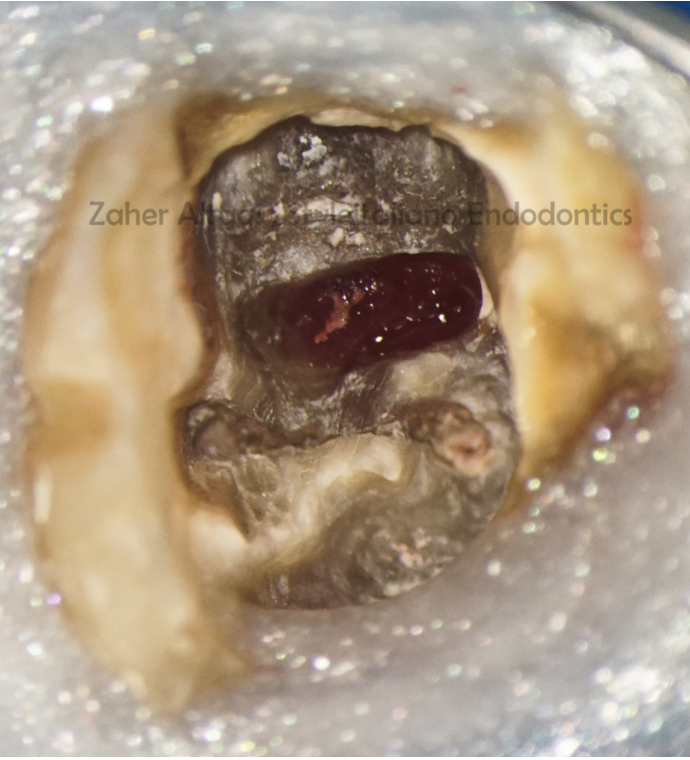
Fig. 4
All restorative material was carefully removed with ultrasonic tips under high magnification , then a clear view of the perforation could be obtained.

Fig. 5
Retreatment was initiated with gutta-percha removal and orifices relocation.

Fig. 6
2.5% NAOCL was used to clean the perforation area

Fig. 7
With high magnification we can notice the formation of the granulation tissues invading the perforation site coronally. This tissue should be removed before MTA repair by manual excavation and Ca(OH)2 dressing for 2-3 days.

Fig. 8
Clinical image showing the difference after excavation and 3 days of Ca(OH)2.
Clean perforation with no granulation tissue.
Now the perforation is ready to be sealed and repaired by MTA or any other biocompatible material.
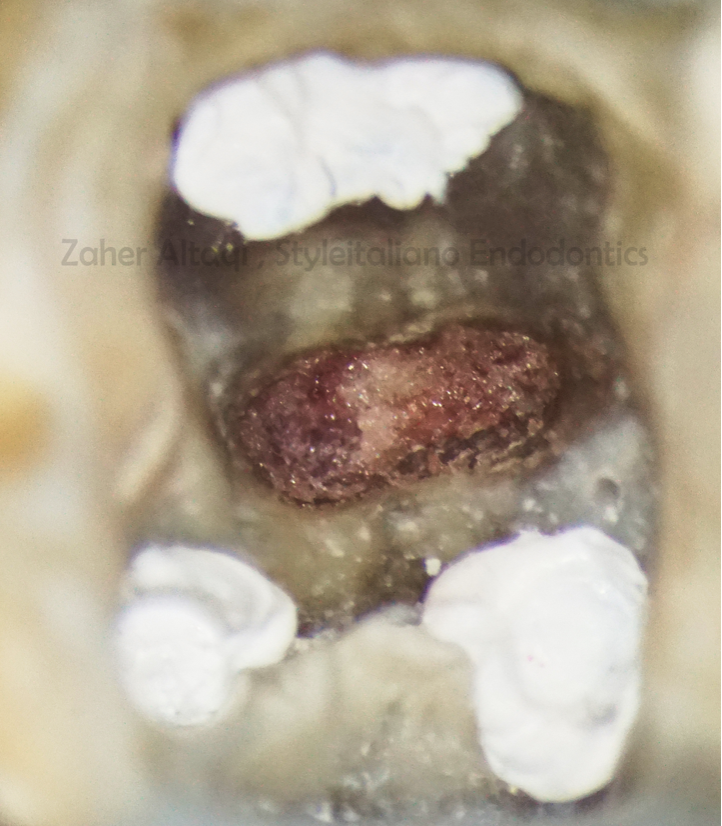
Fig. 9
Before MTA placement, Sponge matrix is used outside the perforation in order to prevent MTA extrusion to the furcal space.

Fig. 10
MTA was packed gently in the perforation site and adapted with pluggers, paper points and micro brushes.

Fig. 11
MTA adaptation with micro brush.
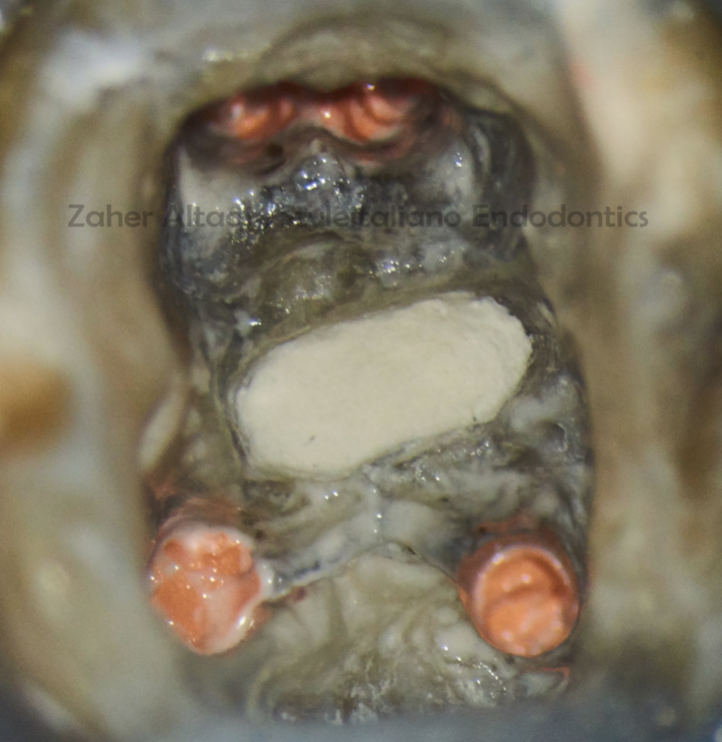
Fig. 12
Complete root canal treatment and obturation with CWC technique after MTA setting.

Fig. 13
Post op radiograph showing the RCT, MTA perforation repair and the final restoration with fiber post and resin core.

Fig. 14
1 Year recall showing good healing in the furcal and apical areas.
Conclusions
It is essential the clinician recognises when a perforation has occurred and has knowledge of the best strategy for correcting the damage. A referral to a more experienced colleague may result in a delay in treatment, which may have serious impact upon the outcome of treatment, therefore, all clinicians should consider immediate repair with the appropriate materials. Patients must be informed that long standing perforations may be unpredictable to repair and consent must include the risks and benefits of either leaving the tooth un repaired or extraction and prosthetic replacement .
Bibliography
1.Gorni FG, Andreano A, Ambrogi F, et al. Patient and clinical characteristics associated with primary healing of iatrogenic perforation after root canal treatment: results of a long-term Italian study. J Endod. 2016;42 (2):211-215.
2. American Association of Endodontists. Treatment Options for the Compromised Tooth: A Decision Guide .
3. Roda RS, Gettleman BH. In: Hargreaves KM, Cohen S, Berman LH, eds. Cohen’s Pathways of the Pulp. 10th ed. St. Louis, MO: Mosby Elsevier:941-942.