Autotrasplantation: from 2.8 to 2.6 with a bioreplica of the original tooth
21/07/2025
Fellow
Warning: Undefined variable $post in /home/styleendo/htdocs/styleitaliano-endodontics.org/wp-content/plugins/oxygen/component-framework/components/classes/code-block.class.php(133) : eval()'d code on line 2
Warning: Attempt to read property "ID" on null in /home/styleendo/htdocs/styleitaliano-endodontics.org/wp-content/plugins/oxygen/component-framework/components/classes/code-block.class.php(133) : eval()'d code on line 2
Autotransplantation is a clinical option that allows us to preserve function, maintain bone, and use a patient’s own tooth as a biological replacement when extraction is unavoidable.
It offers unique advantages when performed under the right conditions and with proper case selection.
Preserving the periodontal ligament during extraction is critical, as it plays a central role in the healing process. The timing of endodontic treatment is also essential, as early intervention can interfere with tissue regeneration, while delayed treatment allows for better periodontal repair. Splinting should be light and flexible, allowing slight functional movement that allows natural healing and prevents ankylosis.
This biological approach requires a delicate balance between surgical precision and respect for the body’s ability to heal itself.
In this case, we treated a patient with a fractured upper first molar, which was not restorable. A third molar with complete root formation was chosen as the donor and was atraumatically extracted and placed in the 2.6 socket. A flexible splint was used for two weeks, after which endodontic treatment was performed and the splint removed.
This treatment choice was based not only on clinical feasibility, but also on the desire to preserve natural tissue and avoid more invasive prosthetic or implant-based options.
When performed carefully, autotransplantation can become a reliable and biologically sound alternative, with the potential for long-term stability and success.
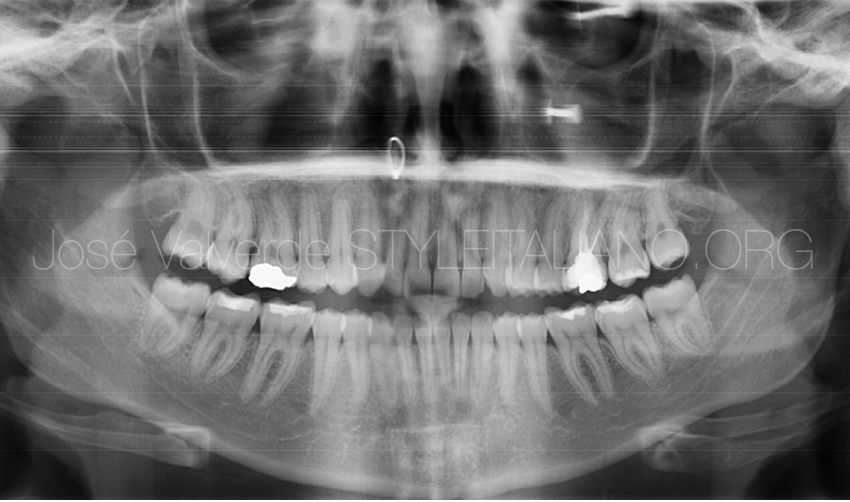
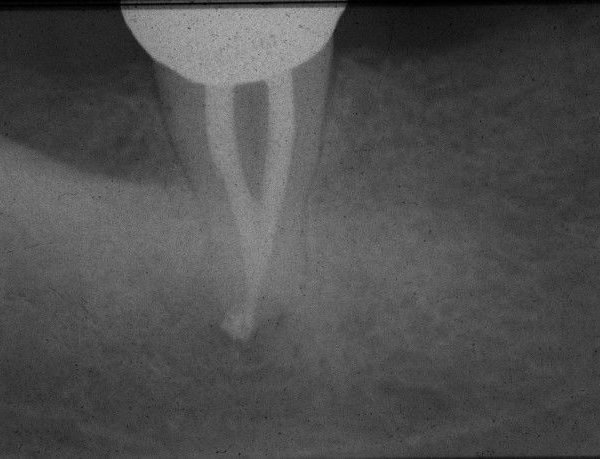
Fig. 1
A 22-year-old female patient came to the clinic concerned about pain in the second quadrant.
The X-ray showed that tooth 2.6 had endodontic treatment with an apical lesion. Clinical examination revealed a fracture and that the tooth was not restorable.
Upon further analysis of the X-ray, we see that tooth 2.8 is intact and has a conical root, making it an ideal candidate for autotransplantation.
The patient has no systemic diseases or pathologies.
We take a CBCT scan to plan the case and make a replica of tooth 2.8.

Fig. 2
Image of the initial situation in the second quadrant of the patient.
Tooth 2.6 has been previously treated and has a coronal fracture.
Tooth 2.8 is intact, with only stained grooves, but after analyzing the CBCT and confirming that its root is conical, we see that it is a candidate for transplantation.
The patient's overall hygiene is good and she has no periodontal problems.
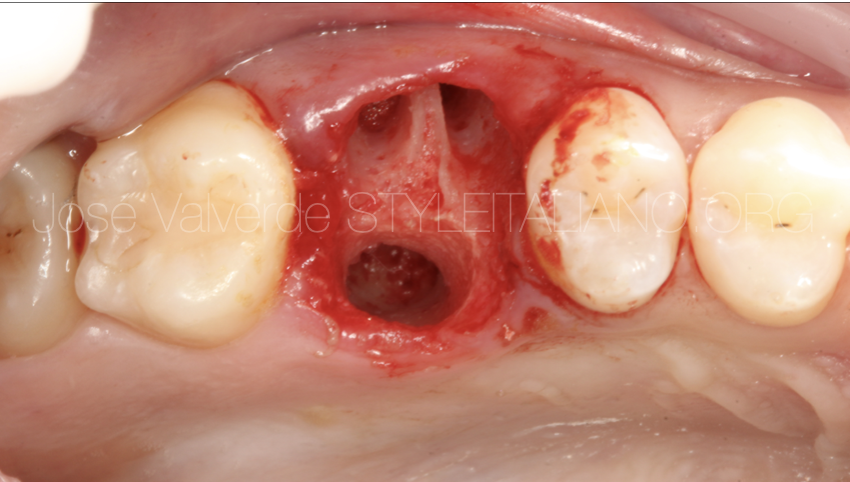
Fig. 3
After extraction of tooth 2.6, the alveolus was prepared by removing the septum to adapt it to the conical shape of the bioreplica.

Fig. 4
In this image, we can see tooth 2.8, which has just been extracted, alongside its replica.
The extraction was performed in an atraumatic manner to preserve as much healthy periodontal ligament as possible.

Fig. 5
After extracting tooth 2.6, the alveolus was prepared to fit the bioreplica. This way, we avoided testing tooth 2.8 in the alveolus, which would have damaged the healthy periodontal ligament fibers.

Fig. 6
Fitting confirmation of tooth 2.8 in the previously prepared alveolus with the bioreplica

Fig. 7
The occlusion was adjusted after tooth 2.8 was placed in the alveolus of 2.6, and flexible splinting of the donor tooth to the adjacent teeth was performed. This splinting was maintained for one month.

Fig. 8
After two weeks, root canal treatment was performed on donor tooth 2.8.
As we had the CT scan information, we were able to plan a conservative access to make the most of the tooth structure, which was intact and free of caries.
The treatment was performed with splinting, as we planned to keep it in place for one month due to the modification of the receiving socket.
The case was treated with BlueShaper Pro from Zarc, and the final apical preparation was 25/06 in all canals.
During the treatment, the tooth was irrigated profusely with 4.25% NaOCl using the Irriflex irrigation tip from Produitsdentaires.
As a final irrigation, we used sonic activation using 4.25% NaOCl + 17% EDTA. We finished the irrigation with apical negative pressure and cleaning of the canal system with saline solution prior to filling.
Finally, obturation was performed with Zarc NeosealerFlo hydraulic cement and 4% gutta-percha.
The restoration was performed immediately with SDR and Spectra from Dentsply.
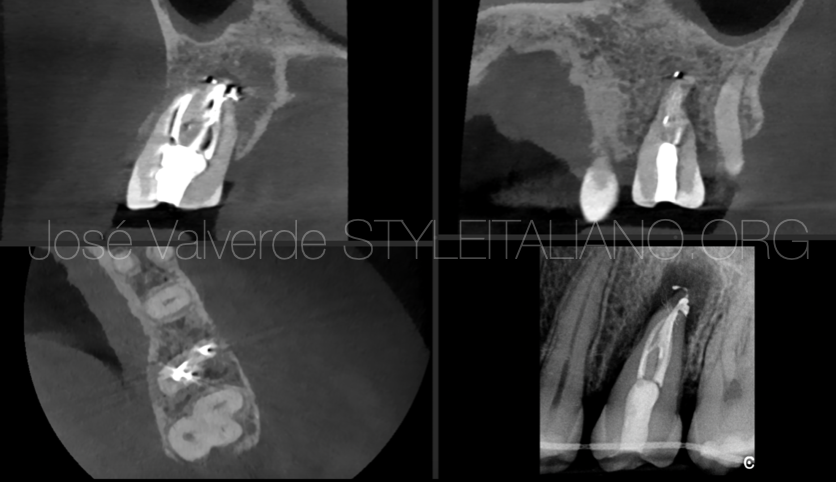
Fig. 9
A final CBCT was performed to verify that we had treated the entire anatomy and to confirm that the position of the donor tooth was optimal. We will use this CBCT for long-term monitoring.
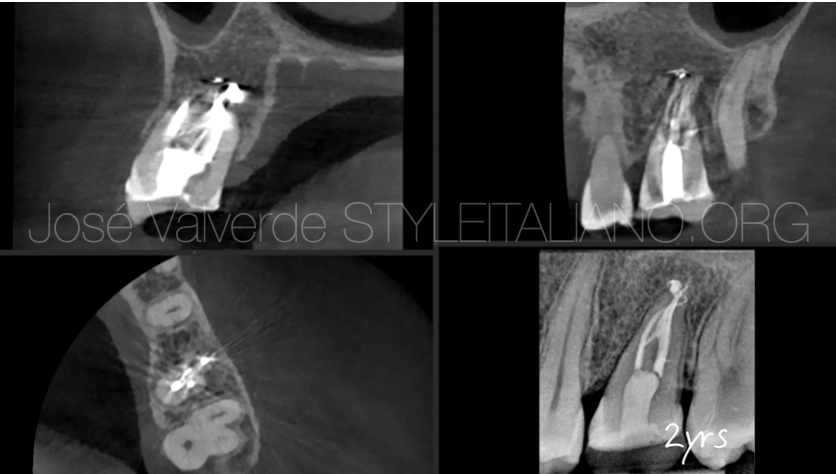
Fig. 10
At the two-year check-up, we see complete healing of the lesion.
After the initial six months of treatment, the patient had a composite onlay placed.
She is completely asymptomatic and the tooth remains stable

Fig. 11
About the author:
José Valverde
- 2009-2014: Graduated in dentistry from the Alfonso X El Sabio University
- 2016-2019: European Master in Microscopic Endodontics and Apical Surgery from the Rey Juan Carlos University
- In 2023 he has started the PhD program in Universidade Grande Rio
- Proffesor of the Master in Microscopic Endodontics and Apical Surgery at Rey Juan Carlos University
- Proffesor of the Expert in Endodontics and Apical Surgery at Universidad La Salle
- Titular Member of the Spanish Association of Endodontics (AEDE)
- Member of the American Association of Endodontics (AAE)
- Member of the International Association of Dental Traumatology (IADT)
- Fellow Member of Style Italiano Endodontics
- Opinion Leader for Zarc4Endo
- He has been an active participant in national and international endodontic congresses, such as AAE, ESE, AEDE or IFEA.
- He works as exclusive endodontist in Gran Canaria, Spain, and is dedicated to research and education
Conclusions
Autotransplantation, when guided by biological principles and careful clinical planning, can offer long-term success as a conservative alternative to implants or prosthetic solutions.
In this case, the use of a bioreplica played a crucial role in reducing the extra-alveolar time and allowing precise preparation of the alveolus, minimizing trauma to the donor tooth. Not only this but the use of a flexible splinting, the endodontic treatment after two weeks, and a conservative adhesive restoration, contributed to favorable healing and stable function over time.
Two years postoperatively, the transplanted tooth remains asymptomatic and functional, with no signs of pathology. This case highlights how technology, when used to respect biology can enhance the outcomes of complex treatments like autotransplantation.
Bibliography
TSUKIBOSHI, Mitsuhiro. Autotransplantation of Teeth. 2nd ed. Tokyo: Quintessence Publishing, 2002.
CZOCHROWSKA, Ewa M., et al. Survival and pulp regeneration of 180 teeth transplanted in adolescents. Dental Traumatology, 2002.
YOSHINO, Koichi, et al. A retrospective study of autotransplantation of teeth with complete root formation. International Journal of Oral and Maxillofacial Surgery, 2012.
VERWEIJ, J.P., et al. Long-term outcomes and factors influencing success of tooth autotransplantation: a systematic review. Clinical Oral Investigations, 2022.