The fine line between extraction and retreatment: a conservative approach to a compromised premolar — 24-Month Follow-Up
17/07/2025
Fellow
Warning: Undefined variable $post in /home/styleendo/htdocs/styleitaliano-endodontics.org/wp-content/plugins/oxygen/component-framework/components/classes/code-block.class.php(133) : eval()'d code on line 2
Warning: Attempt to read property "ID" on null in /home/styleendo/htdocs/styleitaliano-endodontics.org/wp-content/plugins/oxygen/component-framework/components/classes/code-block.class.php(133) : eval()'d code on line 2
The preservation of structurally compromised teeth remains one of the major challenges in modern endodontics. Extensive loss of hard dental tissue due to caries, resorbtions, previous restorations, or earlier endodontic interventions significantly weakens the remaining tooth structure, increasing the risk of fracture and rendering the long-term prognosis uncertain. In such cases, extraction followed by implant placement is frequently considered the treatment of choice. However, a conservative and biologically oriented approach aimed at maintaining the natural tooth and the surrounding alveolar bone may offer significant benefits.
This young patient was referred to the office for an endodontic assessment of right first maxillary premolar. Following a previous examination by another clinician, based on clinical findings and CBCT scan, extraction of the premolar — considered to have a questionable prognosis — followed by implant placement was proposed.
Following my clinical examination and 3D imaging investigations, a diagnosis of previously treated tooth with asymptomatic apical periodontitis was established. Subjectively, the patient reported no painful sensitivity. Objectively, percussion testing in both vertical and horizontal directions yielded negative responses. There was no pain on biting associated with this tooth and the tooth was not mobile. However, slight discomfort was noted upon palpation of the vestibular mucosa in the area corresponding to the roots. Periodontal probing depths around the tooth were within normal limits.
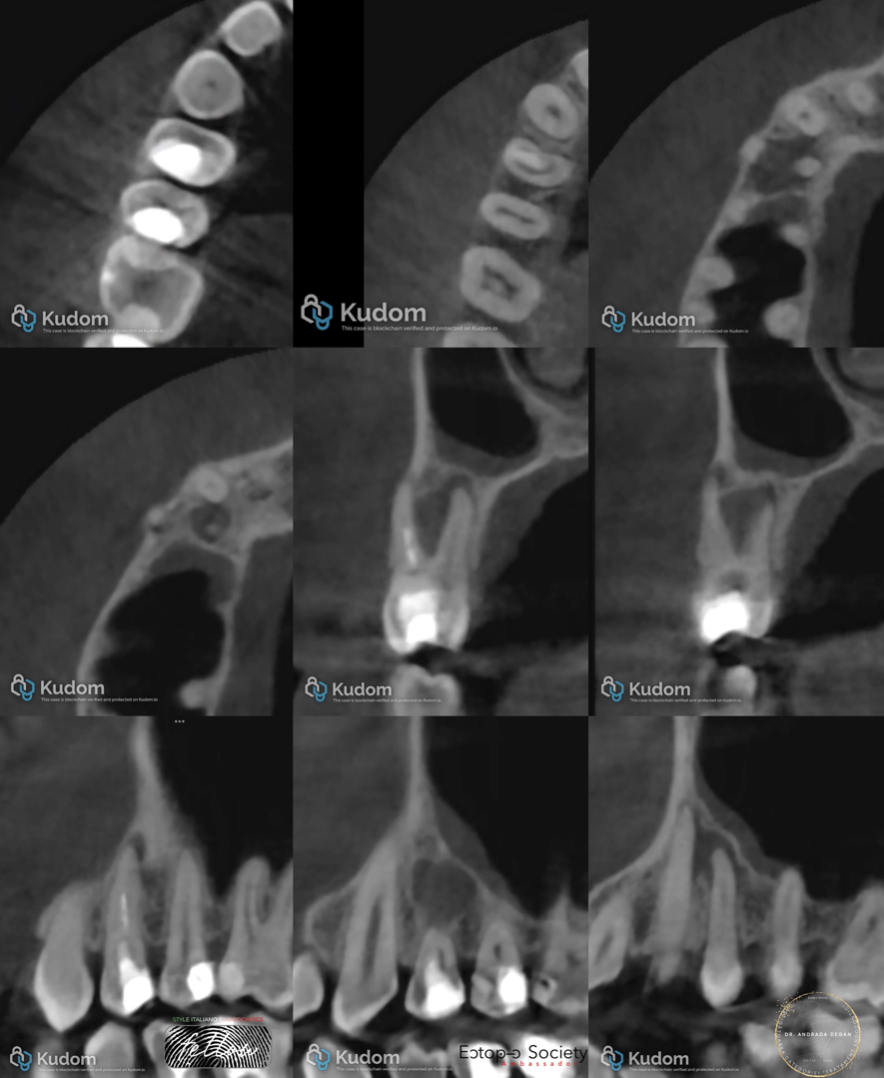
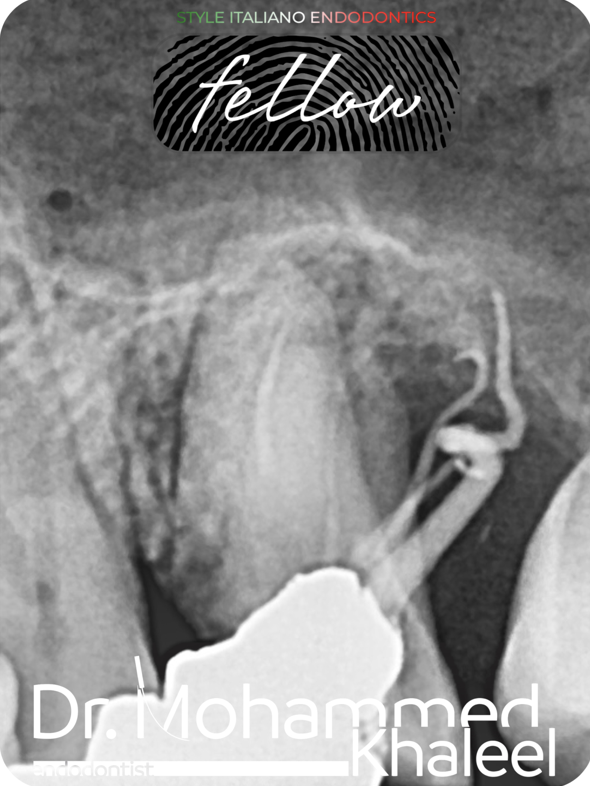
Fig. 1
The preoperative CBCT scan revealed, at the coronal level of upper first premolar, a radiopacity indicating an existing direct restoration, as well as a radiolucent area associated with secondary caries. Additionally, the root canals exhibited an incomplete and non-homogeneous root filling, indicating inadequate canal preparation and disinfection during the prior treatment. As a consequence, a periapical radiolucency is present, extending to the furcation area of the premolar and partially involving the periodontal space of the adjacent canine.
The appearance and extent of the lesion also raise the possibility of a root fracture or crack — a critical factor in the decision-making process regarding treatment versus extraction.
The patient was informed of the questionable prognosis, but we agreed to attempt to save the tooth and monitor it periodically to assess bone remineralization. Furthermore, in the event of a favorable healing response, sufficient bone tissue will be obtained to allow for future implant placement, considering the potential for fracture or failure due to the insufficient thickness of the remaining tooth structure.

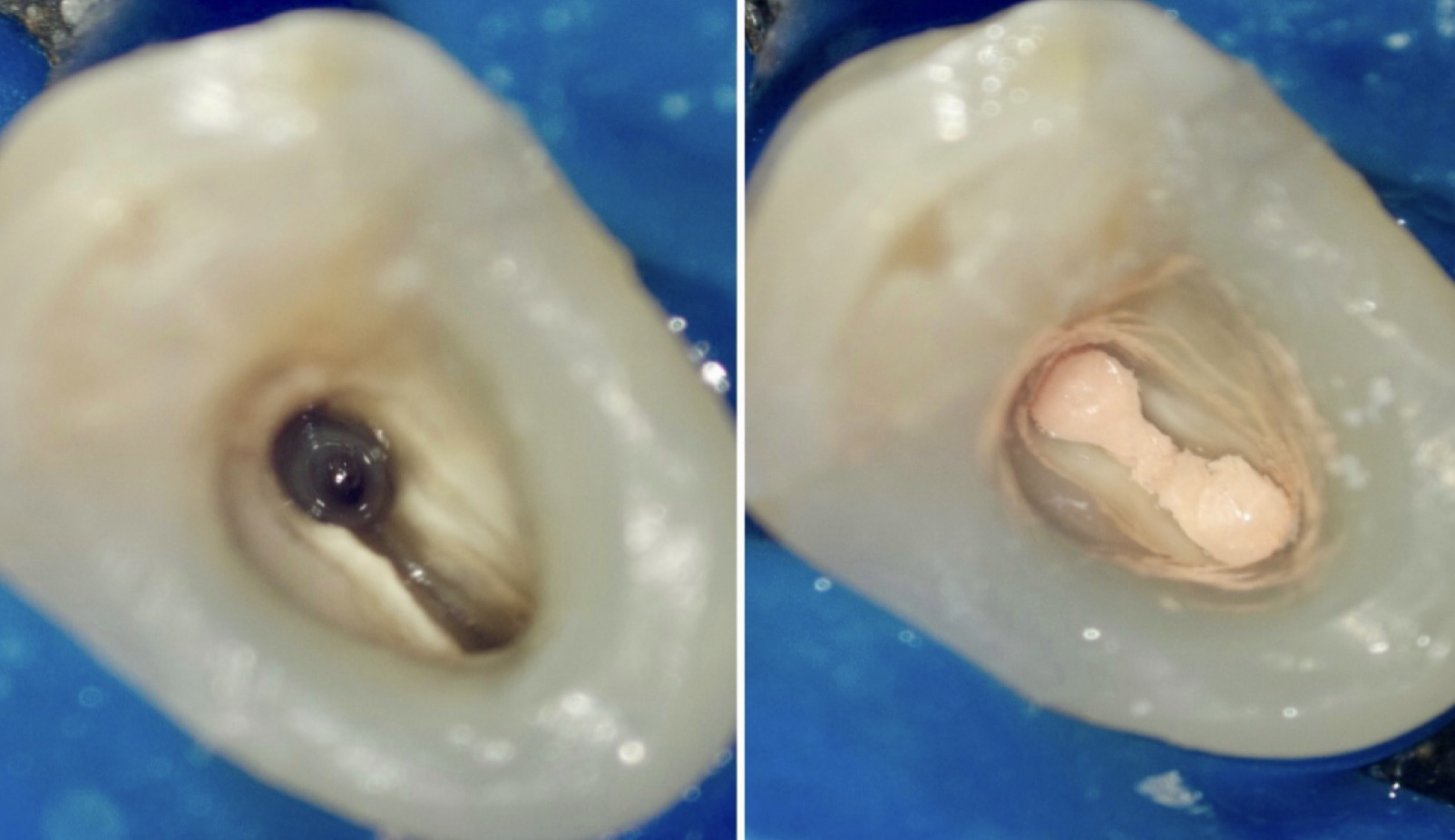
Fig. 2
Upon removal of the restoration, a large area of infected dentine was found which had compromised a significant amount of hard dental tissue, thus jeopardizing the structural integrity of the premolar. Complete removal of the infected dentine resulted in a perforation in the mesial cervical area.
The American Association of Endodontists (AAE) defines perforation as a mechanical (access perforation, post drilling errors) or pathological (resorptions or caries) communication between the root canal system and the external surface of the tooth. In this case, the primary cause was extensive dental caries.
The position of the perforation and the time elapsed before it is sealed are critical determinants of the treatment outcome. Perforations located near the gingival sulcus present a less favorable prognosis due to a higher risk of microbial contamination. Delayed management may allow epithelial tissue to migrate apically, potentially resulting in periodontal breakdown. The size of the perforation also significantly influences the prognosis, with larger defects being more challenging to seal and more likely to compromise healing.
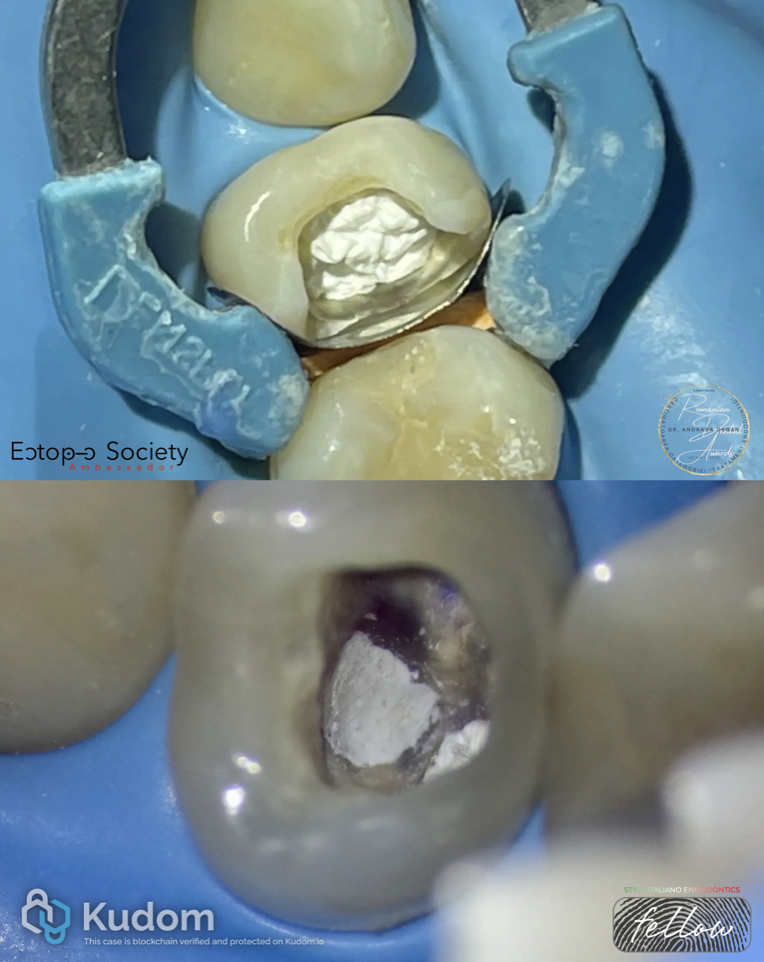
Fig. 3
The perforation was repaired in the same session of treatment, using white MTA (Angelus). Bioactive materials like mineral trioxide aggregate (MTA) and other calcium silicate-based cements have demonstrated success in managing perforations by creating a regenerative-friendly environment.
The treatment was carried out in two sessions. In the first appointment, a pre-endodontic build-up was performed, protecting the pulp chamber with a sterile teflon pellet. Subsequently, the mineral trioxide aggregate was delivered into the perforation site using an MTA carrier and gently compacted with sterile paper points with trimmed tips.
A moistened cotton pellet was placed over the bioceramic material to facilitate its setting, and the access cavity was temporarily sealed until the next appointment using a glass ionomer cement.
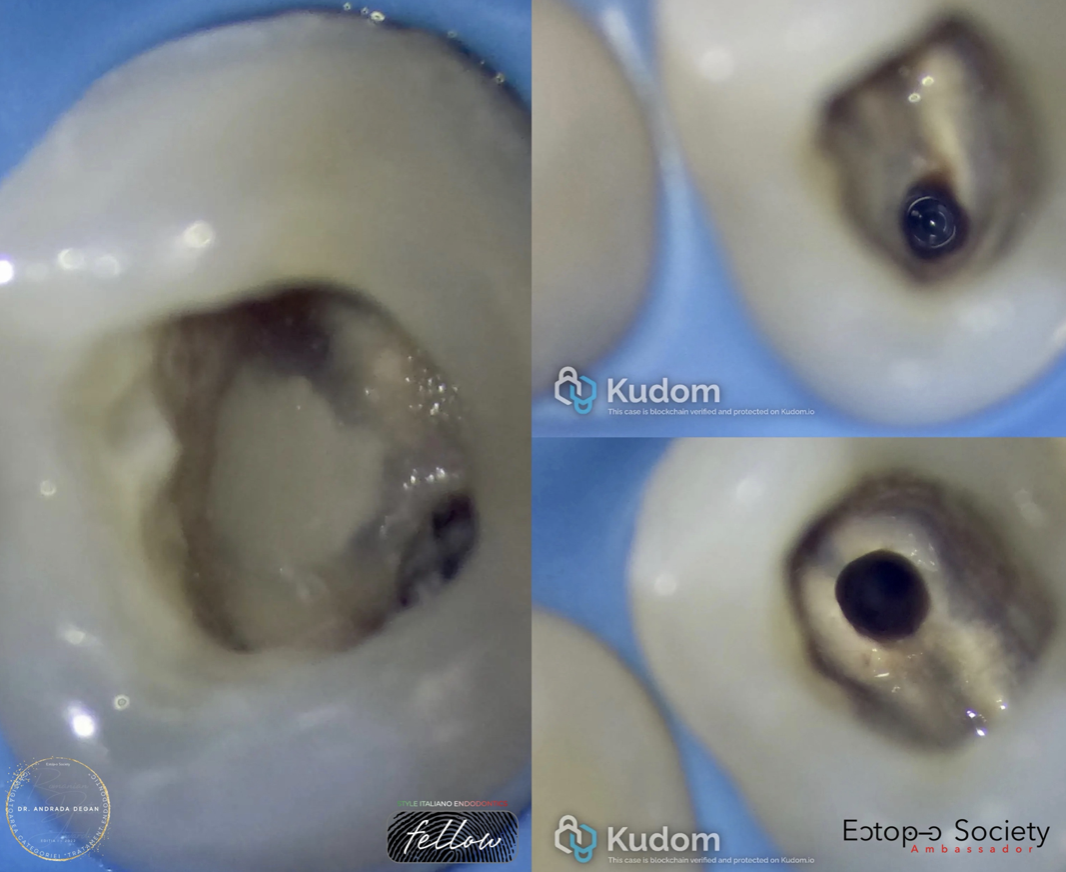
Fig. 4
Until the second session, the material had set, and during this appointment, treatment was continued. The MTA repair site was sealed with flowable composite, after which the root canal filling materials were removed using a 25/06 NeoNITI (Neolix) rotary file and ultrasonically activated U-files to eliminate residual sealer from the canal walls.
After the removal of the root canal filling materials, working length was determined using a D-Finder (Mani) manual ISO size 10 file and electronic apex locator, measuring 19 mm for the palatal canal and 21 mm for the buccal canal.
The root canals were shaped using a sequence of NeoNiTi (Neolix) rotary instruments: 15/03, 20/06, 25/06, and 30/04. Apical gauging was established at ISO size 35 for both canals. A 5.25% sodium hypochlorite solution was used for irrigation between instrumentation steps. No cracks or fractures at the level of root canal walls were noticed under magnification during this step.
The final disinfection protocol of the endodontic system consisted of irrigation with approximately 10 ml of 5.25% sodium hypochlorite solution and 2 ml of 17% EDTA solution per canal, with ultrasonic activation for 30 seconds after each irrigation cycle of about 1 minute. Saline was used as a final rinse. The root canals were dried using paper points and obturated using the warm vertical compaction technique.

Fig. 5
This figure shows the final periapical radiograph taken before direct restoration. Given the guarded prognosis, we opted for a direct composite restoration, with the plan to reassess the tooth's structural and biological integrity before committing to a more definitive prosthetic restoration.

Fig. 6
At the 12-month follow-up, a small field-of-view CBCT scan was performed to obtain an accurate assessment of the lesion status. Given the interradicular extension of the lesion, a conventional periapical radiograph would not have provided the same level of diagnostic detail. Additionally, the use of CBCT allowed for a direct comparison with the preoperative imaging of the same type. The scan revealed signs of ongoing healing. The patient reported no symptoms, and periodontal probing depths remained within normal limits.

Fig. 7
At the 24-month follow-up, the lesion appeared to be almost completely healed. The patient reported no discomfort, and periodontal probing depths remained within normal limits.
Studies indicate that nonsurgical root canal treatment can lead to complete healing in a significant percentage of cases with large periapical lesions. While some lesions heal quickly, others may take longer. Research suggests that only half of eventually healed lesions show signs of healing at the 6-month mark, with 88% showing signs at 12 months, and complete healing can take up to four years in some cases.
Given the current clinical situation, a cuspal coverage restoration was recommended to prevent a potential fracture of the premolar.

Fig. 8
About the author: Dr Andrada Maria Degan
Dr. Andrada Maria Degan graduated from the Faculty of Dental Medicine at the University of Medicine and Pharmacy in Târgu Mureș, later becoming a Specialist in Endodontics following her residency program in Cluj-Napoca.
She holds a Master’s Degree in Advanced Endodontics, awarded by the University of Siena, Italy.
She was the winner of the first edition of the Romanian Dental Awards in the “Endodontic Treatment” category, and shortly thereafter became an ambassador of the Ectopic Society.
Following an endodontic bootcamp held during the 3rd International Style Italiano Endodontics Congress in Athens, she won the “Curvy” category, which led to her becoming a fellow of Style Italiano Endodontics.
Currently, her practice is limited to endodontic therapy under magnification and she works in a clinic located in Cluj-Napoca, Romania.
Conclusions
This case demonstrates that even in the presence of a large periapical lesion with interradicular extension and a perforation in a structurally compromised tooth, healing can be achieved through meticulous diagnosis, proper disinfection, and the use of modern bioactive materials. The successful repair of the perforation—despite its location near the gingival sulcus, a site generally associated with a less favorable prognosis—highlights the regenerative potential of calcium silicate-based cements such as MTA.
Furthermore, although the remaining dentinal wall thickness did not exceed 2 mm, the presence of one intact marginal ridge played a critical role in enhancing the tooth’s resistance to fracture. Nevertheless, given the inherent structural vulnerability, a cuspal coverage restoration is strongly recommended in the future to ensure long-term mechanical stability and minimize the risk of catastrophic failure.
Bibliography
American Association of Endodontists. (2014). Treatment options: Saving the natural tooth – A guide to clinical decision making
Karamifar, K., Tondari, A., & Saghiri, M. A. (2020). Endodontic periapical lesion: An overview on the etiology, diagnosis and current treatment modalities. European Endodontic Journal, 5(2), 54–67.
Clauder, T. (2022). Present status and future directions – Managing perforations. International Endodontic Journal, 55(S4), 872–891.
Gagliani, M., Gorni, F., & Bertani, P. (Eds.). (2020). Retreatments. Solutions for periapical diseases of endodontic origin. EDRA
Schwartz, R. S., Mauger, M., Clement, D. J., & Walker, W. A. (2014). Treatment outcome of mineral trioxide aggregate: Repair of root perforations—Long-term results. Journal of Endodontics, 40(6), 790–796
Scotti, N., Rota, R., Scansetti, M., Paolino, D. S., Chiandussi, G., Pasqualini, D., & Berutti, E. (2013). Influence of adhesive techniques on fracture resistance of endodontically treated premolars with various residual wall thicknesses. The Journal of Prosthetic Dentistry, 110(5), 376–382.
Mannocci, F., & Cowie, J. (2014). Restoration of endodontically treated teeth. British Dental Journal, 216(6), 341–346.
Cohen, S., Hargreaves, K. M., & Berman, L. H. (Eds.). (2021). Cohen’s pathways of the pulp (12th ed.). Elsevier.