Surgical management of Chronic Apical Periodontitis Due to an untreated Lateral Canal: A case report with 6-Month Radiographic Follow-Up
14/12/2024
Fellow
Warning: Undefined variable $post in /home/styleendo/htdocs/styleitaliano-endodontics.org/wp-content/plugins/oxygen/component-framework/components/classes/code-block.class.php(133) : eval()'d code on line 2
Warning: Attempt to read property "ID" on null in /home/styleendo/htdocs/styleitaliano-endodontics.org/wp-content/plugins/oxygen/component-framework/components/classes/code-block.class.php(133) : eval()'d code on line 2
Even with proper treatment, a tooth may develop a periapical lesion. Periapical lesions may also arise from incomplete cleaning and sealing of lateral canals, with the prevalence in such cases reported to vary in the literature. In cases where the tooth has a prosthetic restoration or a very thin root, such as an upper second premolar, surgical endodontics may provide a valid alternative.
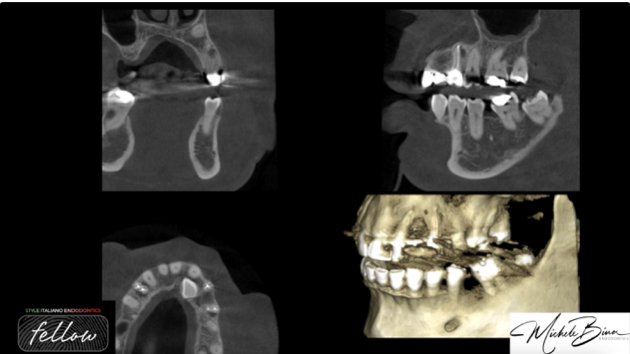
Fig. 1
A 50-year-old female patient presented with pain during chewing associated with tooth 24. Upon clinical examination, the tooth showed a positive response to percussion testing with no pathological periodontal probing depths. CBCT imaging revealed a radiolucent area at the middle third of the distal root of tooth 24.
Based on clinical and radiographic findings, the diagnosis was chronic apical periodontitis caused by an untreated lateral canal. Considering the presence of a prosthetic crown on the tooth, a surgical approach was deemed the most appropriate treatment option.

Fig. 2
In the two-dimensional radiograph, a periodical radiolucency is clearly visible, consistent with the findings observed in the CBCT imaging
Surgical Procedure
The surgery was performed under local anesthesia using 1:50,000 lidocaine to ensure profound anesthesia and achieve optimal intraoperative hemostasis. A full-thickness mucoperiosteal flap with a mesial releasing incision was carefully elevated to gain adequate access to the treatment area while minimizing trauma to surrounding tissues.
Using preoperative CBCT data, the surgical site was meticulously planned to ensure precision and minimize invasiveness. Osteotomy was performed using the OT5a insert on the Piezosurgery device, which, through its cavitation effect, provided excellent hemostasis and precise bone removal. A minimally invasive cavity was created at the apex of the distal root, exposing the untreated lateral canal.
The position of the lateral canal, as observed on the CBCT scan, was located palatally. Consequently, I slightly beveled the root surface to enhance visualization and provide direct access to the exit of the untreated lateral canal, allowing for its thorough management and sealing.
Retropreparation was performed using ultrasonic tips, creating a cavity suitable for sealing. The canal was subsequently sealed with a premixed bioceramic putty cement known for its excellent sealing properties and biocompatibility. After thorough irrigation of the surgical field with sterile saline, the flap was repositioned and sutured with resorbable 6-0 PGA sutures to ensure a secure closure.

Fig. 3
The 6-month follow-up, radiographic imaging demonstrated complete healing of the periapical lesion, with no signs of residual pathology. The patient reported the resolution of symptoms, with no further complaints of pain or discomfort.

Fig. 4
Postoperative Follow-Up
The 6-month follow-up, radiographic imaging demonstrated complete healing of the periapical lesion, with no signs of residual pathology. The patient reported the resolution of symptoms, with no further complaints of pain or discomfort.

Fig. 5
About the Author:
Michele Bina
Graduated with honors from the University of Cagliari in 2013, Dr. Michele Bina completed a Master’s degree in Clinical Endodontics at the same university in 2015. Since 2016, he has served as a tutor for the aforementioned program. In 2024, he earned a Master’s degree in Oral Surgery from the University of Padua.
Dr. Bina is a member of the Italian Academy of Endodontics, a fellow of Style Italiano, and an opinion leader for Simit. He practices privately in Cagliari, specializing in endodontics, restorative dentistry, prosthodontics, and oral surgery.
Conclusions
This case highlights the challenges of managing apical periodontitis caused by untreated lateral canals, which can compromise the success of root canal therapy even when performed to a high standard. CBCT imaging played a critical role in diagnosis and treatment planning, allowing precise localization of the lesion and detailed surgical preparation.
Surgical endodontics offers a predictable solution for cases where nonsurgical retreatment is not feasible, particularly in teeth with prosthetic restorations or thin root structures. The use of bioceramic materials has further improved the outcomes of retrograde filling procedures due to their biocompatibility, antibacterial properties, and ability to stimulate periapical tissue healing.
Surgical endodontics remains a valid alternative when conventional retreatment is contraindicated or impractical, especially in cases involving prosthetic restorations or challenging root anatomy. This case underscores the importance of advanced imaging, meticulous surgical technique, and the use of biocompatible materials to achieve favorable outcomes.
Bibliography
1.Ng YL, Mann V, Gulabivala K. “A prospective study of the factors affecting outcomes of non-surgical root canal treatment: part 1: periapical health.” International Endodontic Journal. 2011;44(7):583–609.
2.Ricucci D, Siqueira JF Jr. “Challenges to achieving success in endodontics: A case report.” Journal of Endodontics. 2008;34(10):1249–5
3. Low KM, Dula K, Bürgin W, von Arx T. “Comparison of periapical radiography and limited cone-beam tomography in posterior maxillary teeth referred for apical surgery.” Journal of Endodontics. 2008;34(5):557–62.